Understanding Pancreatitis and Its Symptoms
Pancreatitis is a condition that occurs when the pancreas, a vital organ responsible for producing digestive enzymes and hormones like insulin, becomes inflamed. This inflammation can lead to various complications and severe stomach pain, making it crucial to understand the link between the two. In this section, we will delve into the symptoms of pancreatitis and how they manifest in the body.
Common symptoms of pancreatitis include severe abdominal pain, nausea, vomiting, fever, rapid pulse, and weight loss due to a lack of appetite. The pain is usually felt in the upper middle or left part of the abdomen and often radiates to the back. In some cases, the pain worsens after eating or during nighttime hours. It is important to recognize these symptoms early on, as untreated pancreatitis can lead to severe complications and even death.
Types of Pancreatitis: Acute and Chronic
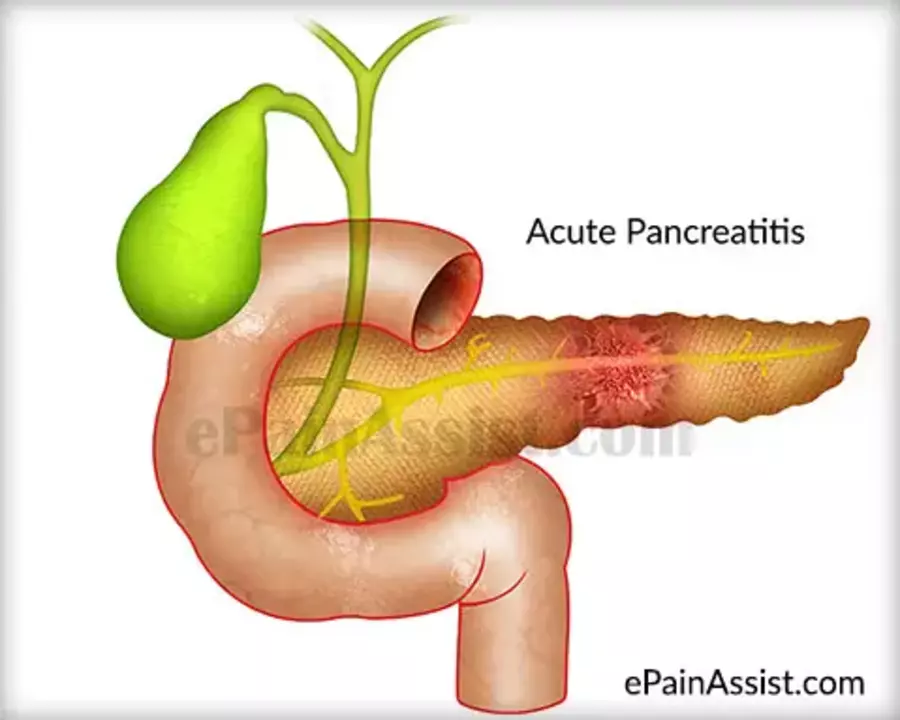
There are two main types of pancreatitis: acute and chronic. Acute pancreatitis is a sudden inflammation of the pancreas, which usually resolves within a few days or weeks. It can be mild or severe, with severe cases sometimes leading to life-threatening complications. The causes of acute pancreatitis include gallstones, excessive alcohol consumption, certain medications, and high triglyceride levels.
Chronic pancreatitis, on the other hand, is a long-lasting inflammation that occurs over an extended period. The pancreas becomes scarred and loses its ability to function properly, leading to malabsorption of nutrients and the development of diabetes. Common causes of chronic pancreatitis include long-term alcohol abuse, hereditary factors, and autoimmune conditions.
Diagnosing Pancreatitis: Tests and Procedures
To diagnose pancreatitis, doctors will first take a detailed medical history and perform a physical examination to assess the severity of the abdominal pain. They may also order blood tests to check for elevated levels of pancreatic enzymes, which indicate inflammation of the pancreas.
Imaging tests, such as abdominal ultrasound, CT scan, or MRI, may also be used to visualize the pancreas and identify any abnormalities, such as swelling or fluid collections. In some cases, an endoscopic ultrasound (EUS) may be necessary to get a closer look at the pancreas and surrounding organs. A biopsy may be taken during EUS to confirm the diagnosis and rule out other possible causes of the abdominal pain.
Treatment Options for Pancreatitis
The treatment of pancreatitis depends on the severity and type of the condition. For mild cases of acute pancreatitis, supportive care, including fasting, pain relief, and intravenous fluids, may be sufficient to help the pancreas heal. In more severe cases, hospitalization may be necessary to monitor and manage complications, such as infections or organ failure.
Chronic pancreatitis treatment focuses on managing pain, improving digestion, and addressing complications. This may involve medications to control pain, enzyme supplements to aid digestion, and insulin therapy to manage diabetes. In some cases, surgery may be necessary to remove damaged pancreatic tissue or treat complications.
Preventing Pancreatitis and Reducing Risk Factors
While not all cases of pancreatitis can be prevented, there are steps you can take to reduce your risk factors. Maintaining a healthy lifestyle is crucial, as obesity and high triglyceride levels can increase the risk of developing pancreatitis. This includes eating a balanced diet, getting regular exercise, and maintaining a healthy weight.
Limiting alcohol consumption is also essential, as excessive alcohol use is a significant risk factor for both acute and chronic pancreatitis. Quitting smoking can further reduce your risk, as smoking has been linked to the development of pancreatitis and its complications.
Living with Pancreatitis: Lifestyle and Diet Changes
Managing pancreatitis often requires making lifestyle and dietary changes to support your pancreas's health and prevent further complications. Eating a low-fat, nutrient-rich diet can help reduce the strain on your pancreas by easing digestion. It is also essential to eat smaller, more frequent meals, as this can help regulate blood sugar levels and promote better digestion.
Avoiding alcohol is crucial for those with pancreatitis, as it can worsen the inflammation and lead to further damage. Additionally, staying well-hydrated and managing stress levels can support your overall health and well-being while living with pancreatitis.
Complications of Pancreatitis: Recognizing the Risks
Untreated or poorly managed pancreatitis can lead to various complications, some of which can be life-threatening. One such complication is pancreatic pseudocysts, which are fluid-filled sacs that can form in the pancreas and potentially rupture or become infected. In some cases, surgery may be necessary to drain or remove the pseudocyst.
Other complications of pancreatitis include infection, malnutrition due to the inability to properly digest and absorb nutrients, and diabetes resulting from damage to the insulin-producing cells in the pancreas. In severe cases, pancreatitis can lead to organ failure and even death. Early diagnosis and treatment are crucial to prevent these complications and manage the condition effectively.
Seeking Medical Attention for Severe Stomach Pain
If you experience severe stomach pain or suspect you may have pancreatitis, it is essential to seek medical attention promptly. Early diagnosis and treatment can help prevent complications and allow for a better prognosis. Remember that pancreatitis is a serious condition, and it is crucial to take any symptoms, such as severe abdominal pain, nausea, vomiting, and fever, seriously.
By understanding the link between severe stomach pain and pancreatitis, you can take steps to reduce your risk factors and maintain the health of your pancreas. If you are living with pancreatitis, making lifestyle and dietary changes can help manage the condition and prevent further complications.

Justin Ornellas
May 11, 2023 AT 12:13When the pancreas erupts in flame, the body flails like a ship caught in a tempest; the pain is not merely discomfort but a cosmic indictment of cellular betrayal. The enzymatic onslaught corrodes tissue, turning digestion into a battlefield where every bite is a cannonball. One can trace the pathophysiology from gallstone obstruction to the cascade of cytokines that whisper nihilism into the bloodstream. In acute episodes, the swift administration of isotonic fluids and analgesia is the only lifeline that can tether a patient to sanity. Chronic sufferers, meanwhile, become scholars of their own misery, cataloguing malabsorption, steatorrhea, and the inexorable march toward diabetes. Ignorance of this chain is a tragedy of epic proportion, and the only remedy is rigorous education and early intervention.
JOJO Yang
May 11, 2023 AT 15:00Listen, bro, you cant just waltz into a hospital and expect miracles-your body *needs* respect, not your half‑baked theories about enzymes. If you keep chugging that cheap booze and ignore the red flags, you're basically signing your own death warrant, and that is just plain immoral. Stop acting like you know everything when the facts are staring you in the face!
Seriously, the pancreas isn’t a toy, so treat it like one.
Faith Leach
May 11, 2023 AT 17:46Don't be fooled-big pharma wants you to blame lifestyle while they hide secret pancreatic toxins in processed foods.
Eric Appiah Tano
May 11, 2023 AT 20:33That's a powerful point, and while we should stay vigilant about food additives, the scientific consensus still highlights alcohol and gallstones as the primary culprits for pancreatitis. Maintaining a balanced diet, staying active, and getting regular check‑ups can cut down the risk, regardless of any hidden conspiracies. Remember, empowerment comes from informed choices and reliable sources, not just suspicion.
Jonathan Lindsey
May 11, 2023 AT 23:20Firstly, allow me to extend my deepest condolences to anyone mistakenly believing that a few indulgent meals are the sole arbiters of pancreatic destiny. It is, after all, a marvel of modern medicine that we can now attribute severe abdominal agony to an organ so frequently relegated to the background of culinary conversation. One must appreciate the elegant cascade wherein hypertriglyceridemia, gallstone impaction, and, lest we forget, the ever‑present specter of ethanol consumption orchestrate a symphony of enzymatic havoc. The ensuing inflammation, dear reader, is not merely a localized irritation but a systemic proclamation that the body's homeostasis has been flagrantly violated. Diagnostic protocols, as you are surely aware, involve meticulous serum amylase and lipase quantification-an exercise in biochemical poetry that would make a poet weep with envy. Imaging modalities, ranging from ultrasonography to contrast‑enhanced computed tomography, provide the visual testament to the pancreas's tormented state, rendering any dissenting opinion entirely superfluous. Therapeutic regimens, predicated upon nothing less than aggressive fluid resuscitation, analgesic stewardship, and, when warranted, the judicious use of endoscopic intervention, exemplify the pinnacle of clinical prudence. Chronic afflictions, by contrast, demand an even more austere approach: pancreatic enzyme supplementation, glycemic control, and, for the truly unfortunate, surgical debridement. One cannot overstate the importance of patient education-if a layperson believes that a sprinkling of pepper will magically ameliorate exocrine insufficiency, the resulting disappointment is both inevitable and, frankly, tragic. Moreover, the socioeconomic ramifications of missed workdays, costly imaging, and prolonged hospitalization constitute a fiscal tempest that no insurer wishes to weather. In summation, while it is tempting to romanticize the pancreas as a mere plot device in gastronomic lore, the stark reality is far more sobering. It demands our respect, our vigilance, and-above all-our unwavering commitment to evidence‑based practice. Should you ever encounter a self‑diagnosed 'pancreatic cleanse' on dubious internet forums, remember that such charlatanry is both medically indefensible and legally questionable. Thus, the prudent course remains adherence to professional guidance and a lifestyle that does not tempt the pancreas into rebellion. May your future meals be low‑fat, your alcohol consumption modest, and your medical literature impeccably cited.
Gary Giang
May 12, 2023 AT 02:06Well said, indeed-your eloquent exposition paints the pancreas as a temperamental maestro of the digestive orchestra, and it reminds us all to tread lightly lest we provoke its ire.