- 8
When you walk into a pharmacy in the U.S. and pay $4 for a month’s supply of generic lisinopril, it’s easy to think the system works. But if you’ve ever bought the same pill in Germany or France, you know something’s off - it cost you €15. Meanwhile, the brand-name version of that same drug? In the U.S., it could set you back $500. In Europe? Maybe $120. So why do Americans pay less for generics but way more for brand-name drugs? The answer isn’t about quality, supply, or fraud. It’s about how the systems are built.
The U.S. Generic Market Is a High-Volume, Low-Margin Race
The U.S. generic drug market isn’t just competitive - it’s brutal. Over 90% of prescriptions filled in the U.S. are for generics. That’s higher than any other developed country. Why? Because once a drug loses its patent, dozens of manufacturers jump in. Companies like Teva, Mylan, and Sandoz fight over market share by undercutting each other. Sometimes, they sell pills below cost just to keep their name on the shelf. That’s how prices drop so fast. Pharmacy Benefit Managers (PBMs) - the middlemen between insurers, pharmacies, and drugmakers - drive this even harder. They negotiate rebates by promising huge volumes. A PBM might tell a generic maker: "We’ll send you 10 million pills a month if you give us 40% off." That’s not a discount. That’s a volume deal designed to crush competition. The result? The average U.S. price for a 30-day supply of a generic drug is $28.50. In Europe, it’s $42.10. That’s a 32% difference - and it’s real. But here’s the catch: those low prices aren’t always sustainable. When margins get too thin, manufacturers quit. In 2021, a shortage of generic doxycycline hit hard because three of the four top makers had left the market. One company stepped in, bought up the remaining capacity, and raised prices by 1,200%. That’s the dark side of hyper-competition: prices crash, then spike.Europe’s System Is Built to Keep Prices High - On Purpose
European countries don’t want a race to the bottom. They want control. Most have government agencies that set drug prices directly. In Germany, prices are tied to what other countries pay. In France, they use a fixed reimbursement rate. The UK’s NICE evaluates whether a drug is worth the cost based on health outcomes - not just how much it costs to make. Because of this, only 41% of prescriptions in Europe are for generics - less than half the U.S. rate. Why? Because there’s less pressure to switch. Doctors don’t always substitute generics automatically. Pharmacies can’t swap them without approval. And manufacturers? They don’t need to slash prices to compete. With fewer players and less volume, they can hold onto higher margins. The result? European patients pay more for generics, but they pay far less for brand-name drugs. A 2023 U.S. government report found that Americans pay 422% more for brand-name drugs than Europeans. That’s not because U.S. drugmakers are greedy. It’s because Europe pays less - and the U.S. picks up the tab.
Why the U.S. Pays More for Brand-Name Drugs
The U.S. is the world’s biggest drug market. It makes up 40% of global pharmaceutical sales, even though it has only 4% of the world’s population. That’s not a coincidence. Drug companies know they can charge more here. There’s no central price negotiator. No government agency saying, "This drug isn’t worth more than $200 a month." Instead, you’ve got a patchwork of insurers, PBMs, and hospital systems - all negotiating separately. That means drugmakers can charge one price to Medicare, another to private insurers, and a third to cash-paying patients. The list price you see on the bottle? It’s often meaningless. The real price? That’s buried in rebates. PBMs get 35-40% off list prices from brand-name makers - but patients rarely see that discount. If you’re on Medicare Part D, you pay based on the list price until you hit your deductible. That’s why people get hit with $1,000 bills for a single prescription. Meanwhile, in Germany, the same drug might be priced at $120 - no hidden rebates, no deductible. The price you see is the price you pay. The Inflation Reduction Act tried to fix this. Starting in 2024, Medicare started negotiating prices for 10 high-cost drugs. For Jardiance, Medicare cut the price from $590 to $204. That’s still 3.9 times higher than what other countries pay. But it’s a start. By 2027, 60 drugs could be under negotiation. That could bring U.S. brand-name prices down - but not to European levels.The Hidden Trade-Off: Who Funds Global Drug Innovation?
There’s a bigger picture here. The global pharmaceutical industry spends about $150 billion a year on research. Where does that money come from? Roughly two-thirds of it comes from U.S. sales. That’s according to a 2024 analysis in the Milbank Quarterly. Drug companies don’t make their biggest profits in Europe. They make them in the U.S. That means when Europe negotiates low prices, it’s not just saving money - it’s relying on the U.S. to fund the next breakthrough. A new cancer drug? It was probably tested first in the U.S. because companies could afford to run expensive trials here. A new diabetes pill? Likely developed with U.S. revenue. Dana Goldman, a professor at USC, puts it bluntly: "Europe is free-riding on American innovation." That’s not an accusation. It’s an economic reality. If U.S. prices dropped to European levels overnight, many new drugs might never get developed - or would be delayed by years. That’s why proposals like Trump’s "most favored nation" plan - which would tie U.S. prices to the lowest in the world - are so controversial. If the U.S. cuts its prices, drugmakers will raise them elsewhere to make up the loss. Europe could end up paying more. The global system is interconnected. Change one part, and the whole thing shifts.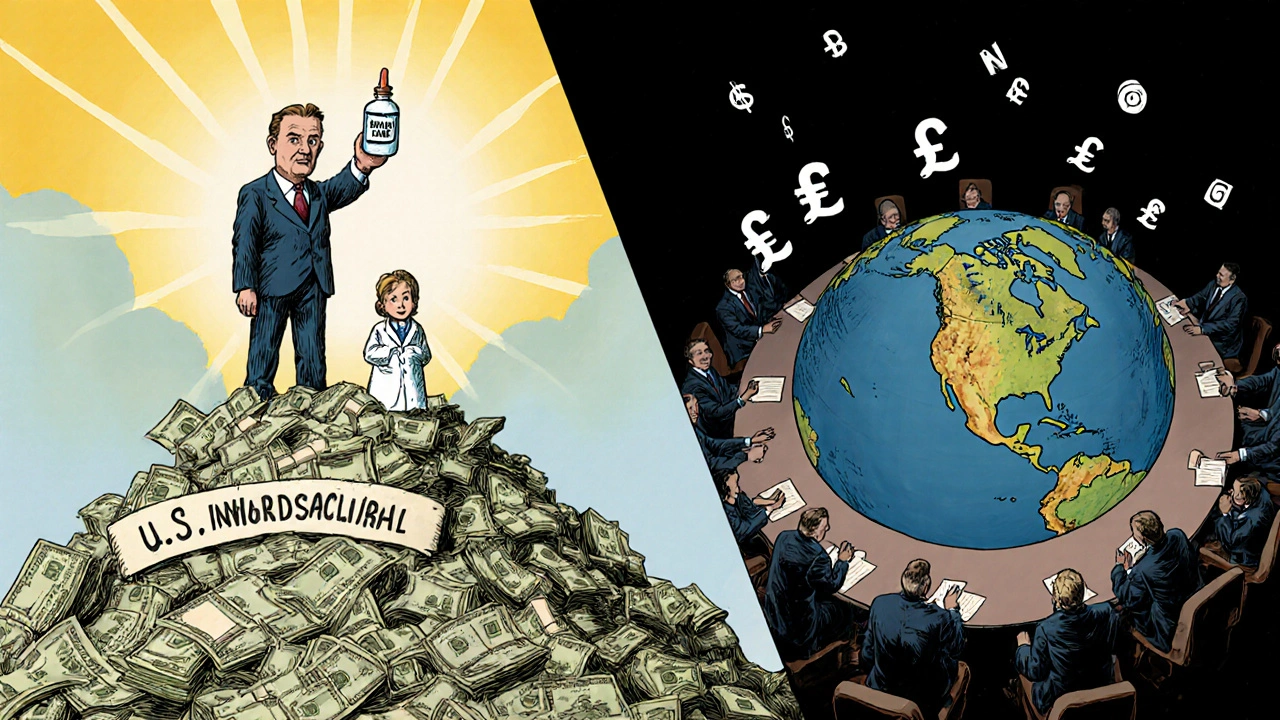


Kezia Katherine Lewis
November 21, 2025 AT 21:48The U.S. generic market operates on a volume-driven, razor-thin-margin model that’s structurally distinct from Europe’s regulated, reimbursement-based framework. PBMs function as oligopolistic intermediaries, leveraging scale to extract rebates that don’t always translate to consumer savings-especially when formulary placement and tiering obscure true cost transparency. The result? A paradox where patients pay less for off-patent molecules but are financially exposed to list-price gouging on branded biologics due to the absence of centralized price negotiation. This isn’t market failure-it’s a policy architecture optimized for pharmaceutical innovation funding, not equitable access.
Laurie Sala
November 23, 2025 AT 12:42Wait-so I’m paying $4 for lisinopril… but if I need my $600 brand-name drug? I’m literally bankrupting my family?!?!!? And you’re telling me Europe pays less for that same drug?!? That’s not capitalism-that’s a moral emergency!!!
Lisa Detanna
November 23, 2025 AT 20:05Look, the U.S. system isn’t broken-it’s just designed to subsidize global R&D. We get cheap generics because we’re the ones footing the bill for the next breakthrough. Europe’s pricing model is sustainable for them, but if we suddenly cap brand-name prices at their levels, we’ll see fewer new drugs come to market. It’s not about greed-it’s about trade-offs. We’ve been the engine of innovation for decades. Now we’re being asked to turn off the engine because others are hitching a free ride. I’m not saying it’s fair, but it’s the reality.
John Mackaill
November 24, 2025 AT 00:39It’s fascinating how the U.S. and EU models reflect deeper cultural attitudes toward healthcare: individual responsibility vs. collective welfare. The U.S. relies on market competition to drive down costs for commoditized goods (generics), while Europe treats pharmaceuticals as a public good requiring state intervention. Neither is perfect. But I’d argue that the U.S. model’s volatility-where prices crash then spike-is inherently more dangerous for patients than Europe’s stable, albeit higher, baseline pricing.
Adrian Rios
November 25, 2025 AT 01:15Let’s be real-this whole system is a Rube Goldberg machine of middlemen, rebates, formularies, and negotiated discounts that nobody understands, not even the pharmacists. You’ve got PBMs taking 35-40% off the list price, insurers paying based on the inflated list price before deductible, patients getting hit with $1,200 bills for a single script, and then-oh, by the way-the manufacturer is secretly paying the PBM a rebate that never reaches the patient. It’s not a market. It’s a shell game. And the only people winning are the ones who designed the game. The Inflation Reduction Act? It’s a Band-Aid on a severed artery. We need a single-payer negotiation system, plain and simple. Anything else is just rearranging deck chairs on the Titanic while people drown from the inside out.
Casper van Hoof
November 25, 2025 AT 17:27One must consider the economic externality inherent in the current pharmaceutical pricing paradigm. The United States, as the largest net importer of pharmaceutical innovation, assumes a disproportionate share of the fixed costs associated with clinical development, regulatory compliance, and post-marketing surveillance. This functionally constitutes a global public good, financed privately by U.S. consumers. The European Union, by contrast, externalizes these costs through centralized price controls, thereby achieving lower per-unit prices at the expense of reduced incentive for marginal innovation. The question is not whether one system is superior, but whether the current equilibrium is sustainable absent structural realignment.
Richard Wöhrl
November 27, 2025 AT 03:51Just to clarify: the 90% generic usage in the U.S. isn’t because patients prefer them-it’s because insurers and PBMs force substitutions. Doctors don’t always have a choice. And when a generic manufacturer exits the market-like with doxycycline in 2021-it’s not just a price spike; it’s a public health crisis. Meanwhile, in Europe, even if the generic price is higher, patients don’t get caught in these wild swings because the government ensures at least two suppliers are always active. Also-big point-when Medicare negotiates, they don’t just cut the price; they negotiate the rebate structure too. That’s why Jardiance dropped from $590 to $204. But here’s the thing: if the U.S. ever caps brand prices too low, companies will just stop launching drugs here first. We’ll get the leftovers. And that’s not innovation-that’s just delayed access.
Pramod Kumar
November 28, 2025 AT 04:56Bro, this whole thing is like a Bollywood drama-everyone’s playing their role, but the script was written by someone who never met a patient. We got cheap generics? Cool. But when your cousin needs that $5K-a-month biologic for lupus, and she’s selling her car to pay for it, that’s not a system-that’s a tragedy wrapped in a spreadsheet. Europe pays more for old pills? So what? At least they don’t make you choose between insulin and rent. The U.S. is like a guy who got the free fries but lost his soul for it. Maybe we need to stop pretending this is about efficiency and start admitting it’s about who gets to live and who gets to wait.