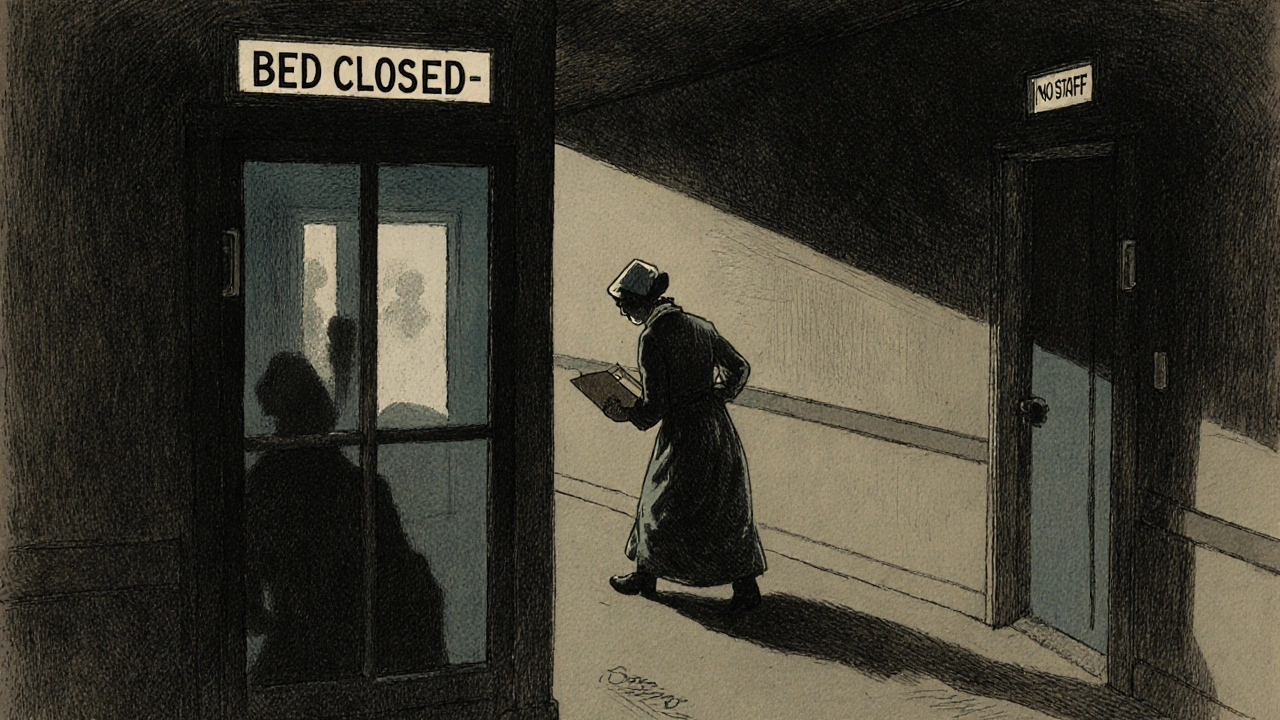
Every day, hospitals and clinics across the U.S. are making impossible choices. Beds are closed because there aren’t enough nurses to staff them. Emergency rooms stretch wait times to over 72 hours. Patients with chest pain wait hours while staff juggle 6 or 7 patients at once. This isn’t a worst-case scenario-it’s the new normal. The healthcare worker shortage isn’t just a headline anymore. It’s breaking the system from the inside out.
Why the Shortage Is Getting Worse, Not Better
The problem didn’t start with the pandemic, but the pandemic made it explode. Before 2020, hospitals were already struggling to fill nursing roles. By 2025, the gap is wider than ever. The Health Resources and Services Administration (HRSA) estimates a shortfall of more than 500,000 registered nurses by 2030. That’s not a guess-it’s a projection based on retirements, burnout, and not enough new nurses coming in to replace them.
Half of all nurses in the U.S. are over 50. That means nearly half the workforce could retire in the next decade. At the same time, nursing schools are turning away over 2,300 qualified applicants each year-not because they lack interest, but because there aren’t enough faculty to teach them. It’s a cycle: no teachers → fewer graduates → more work for existing staff → more burnout → more people leave.
What Happens When There Aren’t Enough Staff
It’s not just longer waits. It’s deadlier care.
Studies show that when nurse-to-patient ratios go above 1:4, patient mortality rates jump by 7%. In emergency departments, understaffing adds 22% more time to patient waits. In rural hospitals, where staffing levels are already 37% lower than in cities, patients are more likely to die from treatable conditions like heart attacks or strokes simply because help arrives too late.
One ICU nurse in Nevada posted on Reddit in April 2025: "I had three patients in my care last night. One was coding. Another was vomiting blood. The third was confused and trying to pull out her IV. I had to choose who to help first. I chose the one who was still breathing." That’s not nursing. That’s triage under siege.
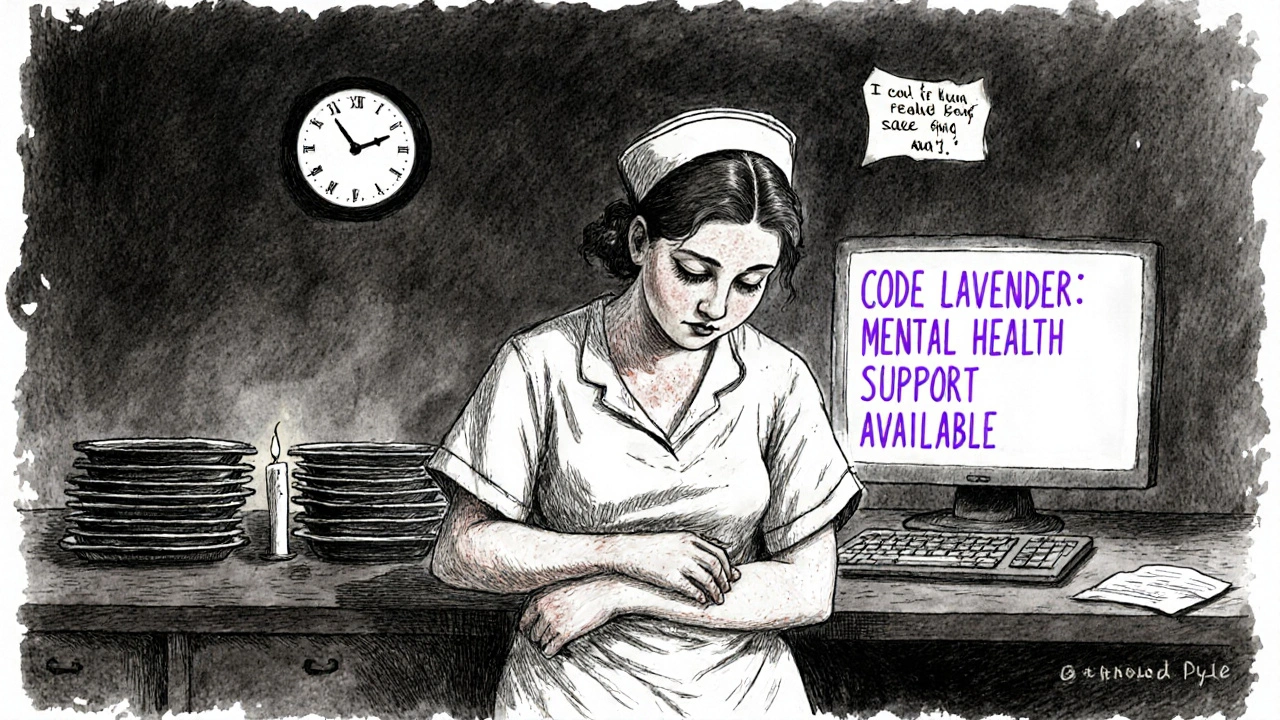
Medication errors are rising. In facilities using mandatory overtime twice a week, staff report a 15% increase in near-miss errors. Hospitals are now hiring "code lavender" teams-mental health responders-for staff who break down from exhaustion. That’s not a support program. That’s a sign the system is failing.
Rural Clinics Are Falling Off the Map
Urban hospitals may have 82% of their nursing positions filled. Rural clinics? Only 58%. That gap isn’t just about distance-it’s about money, training, and isolation.
Small clinics in places like eastern Kentucky or western Nebraska can’t compete with the $185-an-hour pay offered to travel nurses in New York or Los Angeles. Local nurses earn $65 an hour. Why stay when you can make triple the pay and work three weeks a month?
Many rural clinics have shut down their inpatient units entirely. Patients with chronic conditions like diabetes or heart failure now drive 90 minutes for basic check-ups. Some skip care altogether. The result? More ER visits. More hospitalizations. More deaths.

The Band-Aid Solutions That Aren’t Working
Hospitals have tried everything to fill the gaps. Travel nurses. Overtime. AI tools. Cross-training. None of it fixes the root problem.
Travel nurses filled 12% of hospital roles in 2023-but they cost 34% more in wages. That means hospitals are spending more money just to keep the lights on, while permanent staff resent the pay disparity. Some nurses say it feels like the system is rewarding people for leaving, not staying.
AI tools promise to reduce documentation time, but they take 8.7 weeks to learn and require 32 hours of training per clinician. Many older nurses don’t have the digital skills. New hires do-but they’re the ones hospitals can’t hire fast enough.
California tried mandating nurse-to-patient ratios. It helped. But only in places with enough nurses to make it work. In states without the workforce, the rule just forces hospitals to close beds or turn patients away.
What’s Really Needed: Real Fixes, Not Quick Fixes
There are solutions-but they require investment, not just wishful thinking.
First: fund nursing education. The federal government spends $247 million a year on nursing scholarships. Experts say it needs $1.2 billion. That’s a gap of nearly $1 billion. That money could pay for 20,000 new nursing faculty. Each one could train 40 students a year. That’s 800,000 nurses over a decade.
Second: fix licensing. Right now, it takes 112 days on average for a nurse licensed in one state to get approved to work in another. Telehealth could help rural areas-but if nurses can’t cross state lines, it doesn’t matter.
Third: pay nurses like the professionals they are. The American Medical Association says the current wage gap is driving 63% of nurses to consider quitting. If you want people to stay, you have to make staying worth it. That means better pay, better schedules, and real mental health support-not just a 15-minute debrief after a bad shift.
The Human Cost Is Rising Every Day
Behind every statistic is a patient who didn’t get care. A family waiting in an ER for three days. A grandmother with pneumonia sent home because there’s no bed. A nurse crying in the supply closet because she couldn’t save someone.
McKinsey says closing the global healthcare worker shortage could prevent 189 million years of life lost to early death and disability. That’s not a number. That’s mothers, fathers, children, grandparents. People who could have lived longer, better lives-if only there had been enough staff to help them.
We keep talking about "resilience" and "adaptation." But resilience isn’t about working 16-hour shifts. It’s about having enough people so no one has to carry the whole load alone.
The system isn’t broken because of a lack of technology. It’s broken because we stopped valuing the people who keep it running.
Why are hospitals closing beds due to staffing shortages?
Hospitals close beds because they don’t have enough nurses, doctors, or support staff to safely care for patients. For example, a medical-surgical unit needs at least one nurse for every four patients. If only three nurses are on shift, they can’t legally or safely manage more than 12 patients. Any extra beds would be unsafe to use, so they’re shut down to avoid putting patients and staff at risk.
Are travel nurses making the shortage worse?
Travel nurses help fill immediate gaps, but they’re not a long-term fix. They earn significantly more than permanent staff-sometimes over $180/hour-which creates resentment and makes it harder to retain local nurses. They also move frequently, so hospitals can’t rely on them for stable care. Plus, their high cost drains budgets that could be used to hire and support permanent staff.
Can AI or technology solve the staffing crisis?
AI can help with tasks like documentation, scheduling, and remote monitoring-but it can’t replace human judgment in emergencies, emotional support, or complex care. Tools like AI-assisted diagnostics can reduce workload by 20-30% in some areas, but only if staff are trained to use them. Many hospitals lack the time and money to train their teams, and older nurses often struggle with new tech. Technology is a tool, not a cure.
Why aren’t more people becoming nurses?
Nursing school seats are limited because there aren’t enough nursing instructors-over 8.8% of faculty positions are vacant nationwide. Many qualified applicants are turned away. Even when people get in, the workload is overwhelming. Nurses work long hours, face high stress, and often feel undervalued. With burnout rates so high, many leave the field before even graduating.
What’s being done to fix this?
Some states are offering loan forgiveness, expanding nursing programs, and mandating safe staffing ratios. The federal government recently allocated $500 million for nursing education-but experts say that’s only 18% of what’s needed. The American Hospital Association launched a workforce initiative aiming to add 50,000 new workers by 2027. But without major funding increases and policy changes, progress will be too slow to meet demand.
How does this affect patients with chronic conditions?
Patients with diabetes, heart disease, or COPD need regular check-ups and monitoring. With clinic staff stretched thin, appointments are canceled or delayed. Some patients go months without seeing a provider. Their conditions worsen, leading to emergency visits or hospitalizations that could have been avoided. In rural areas, many simply stop seeking care because it’s too hard to get in.
What Comes Next?
The next five years will decide whether the healthcare system recovers-or collapses under its own weight.
If nothing changes, by 2030, 42 states will have nursing shortages so severe that basic care will be unavailable in many communities. Behavioral health services will be nearly nonexistent in rural areas. Emergency rooms will become overflow centers for people who couldn’t get care anywhere else.
The fix isn’t glamorous. It’s not a new app or a fancy robot. It’s paying nurses enough to stay. Training enough teachers so schools can accept more students. Letting nurses work across state lines without waiting months for paperwork. Treating healthcare workers like the lifelines they are-not disposable cogs in a broken machine.
Right now, the system is holding together by sheer willpower. But willpower doesn’t pay bills. It doesn’t heal wounds. It doesn’t bring people back from the edge.
Someone has to decide-before it’s too late-that healthcare workers matter more than budgets.

David Cunningham
November 23, 2025 AT 12:58Man, I’ve seen this in Australia too - rural clinics shutting down, nurses burning out, and the whole system just grinding on fumes. We’re not even talking about a crisis anymore, it’s a slow-motion collapse. And nobody’s doing anything real about it.
Ravi Kumar Gupta
November 25, 2025 AT 07:21Bro this is not just an American problem - in India we have doctors working 3 shifts a week with no breaks and still getting yelled at for not curing cancer in 10 minutes. The world treats healthcare workers like disposable batteries. Charge ‘em up, use ‘em till they die, then throw ‘em out and buy a new one. Pathetic.
Rahul Kanakarajan
November 25, 2025 AT 14:57Oh please. Stop crying. If you can’t handle the stress, go work at a Starbucks. Nursing was never meant to be a 9-to-5 with benefits. You signed up for this. Now stop blaming everyone else for your lack of grit.
Holly Schumacher
November 26, 2025 AT 04:38Actually, the data shows that mandatory overtime increases medication errors by 15%, and 63% of nurses are considering quitting because of systemic disrespect - not because they’re weak. Your ‘grit’ argument ignores the structural violence of underfunding. This isn’t about personal resilience. It’s about capitalism prioritizing profits over human life.
manish chaturvedi
November 27, 2025 AT 01:03Let us not forget that in many developing nations, nurses are the primary caregivers, often without proper equipment, yet they show up every day with dignity. The solution is not just funding - it is global solidarity. We must honor their labor, not just when it’s convenient.
Justin Daniel
November 28, 2025 AT 00:50Y’all are missing the point. The real tragedy isn’t the shortage - it’s that we’ve normalized it. We cheer on nurses like they’re superheroes while refusing to pay them enough to afford rent. That’s not admiration. That’s exploitation dressed up as gratitude.
Jessica Correa
November 28, 2025 AT 18:03i mean like… why are we still surprised? hospitals are run like corporations not care centers. if you treat people like machines you get machine results. nobody wants to work in a place where they’re treated like a cog. duh
james lucas
November 29, 2025 AT 13:23bro i worked in a hospital last year and lemme tell ya, the ai tools they tried to roll out? took 3 months just to get people to stop messing up the login. half the staff was like 55+ and just wanted to do their job without learning a whole new app. and then they got yelled at for not using it right. like… why are we making things harder? just hire more people. it’s not that complicated.
steve o'connor
November 30, 2025 AT 06:22My cousin’s a nurse in Ohio. She quit last month. Said she loved the work but couldn’t stand the guilt of knowing she was letting people down because she was stretched too thin. She’s now driving for Uber. That’s not a win. That’s a national failure.
Nikhil Chaurasia
December 1, 2025 AT 19:48It’s heartbreaking to see how the system rewards those who leave instead of those who stay. The ones who endure the 16-hour shifts, the silent tears, the skipped meals - they’re the ones who get ignored. And the ones who walk away? They get bonuses. It’s backwards.
New Yorkers
December 2, 2025 AT 15:00Let’s be real - the only thing keeping this system alive is the sheer emotional labor of nurses who’ve been conditioned to sacrifice everything. We don’t need more tech. We need to stop pretending that healthcare is a market. It’s a human right. And the people who give their lives for it deserve more than a hashtag.