- 12
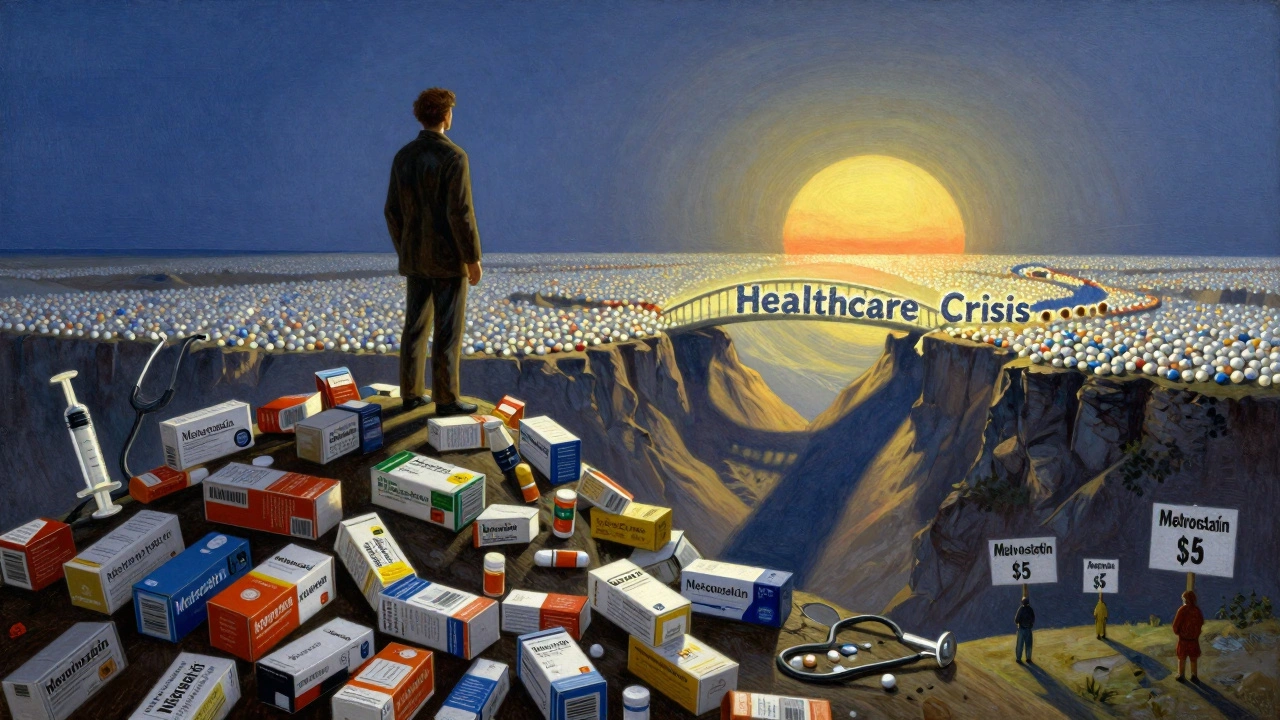
For over a decade, the U.S. healthcare system has quietly avoided a financial collapse-not through sweeping reforms or new taxes, but because millions of people picked up a small, plain pill with a price tag of $4 instead of $400. That’s the power of generic drugs. In 2024 alone, these affordable alternatives saved Americans $467 billion. Over the last ten years, that number added up to $3.4 trillion. That’s more than the entire annual GDP of Canada. And it didn’t come from cutting care. It came from replacing expensive brand-name pills with equally effective generics.
How generics cut costs without cutting corners
Generic drugs aren’t cheap because they’re low quality. They’re cheap because they don’t need to pay for the original research, marketing, or patent protection. Once a brand-name drug’s patent expires, other companies can make the same medicine using the same active ingredients. The FDA requires them to prove they work the same way in the body-same absorption, same strength, same side effects. In practice, that means a patient taking metformin for diabetes pays $4 for a 30-day supply instead of $200. A statin like atorvastatin? $5 instead of $150. The math is simple: 90% of all prescriptions filled in the U.S. in 2024 were generics. Yet they made up only 12% of total drug spending.That’s not a fluke. It’s the result of a 1984 law called the Hatch-Waxman Act, which created a clear path for generic manufacturers to enter the market. Before that, brand-name companies could block competition indefinitely. Afterward, generics started flooding in. By 2024, 3.9 billion generic prescriptions were filled compared to just 435 million brand-name ones. The savings didn’t just help patients. They eased pressure on Medicare, Medicaid, and private insurers. In 2024, generics saved Medicare $142 billion and Medicaid $62.1 billion. That’s money that could go to more nurses, better facilities, or new treatments.
The rise of biosimilars: generics for complex diseases
Not all drugs are simple pills. Some, like those for rheumatoid arthritis, cancer, or multiple sclerosis, are made from living cells. These are called biologics. They’re expensive-sometimes over $1,000 per dose. But in the last decade, a new kind of generic has emerged: biosimilars. These aren’t exact copies (because living cells can’t be cloned perfectly), but they’re close enough to work the same way. The FDA approves them with the same rigor as traditional generics.Biosimilars entered the market slowly. Doctors were cautious. Patients were unsure. But the savings were too big to ignore. By 2024, biosimilars had already saved $56.2 billion since their first approval in 2015. In 2024 alone, they saved $20.2 billion. One biosimilar for the autoimmune drug Humira, for example, cut its price from $7,000 per year to under $3,000. That’s a 57% drop. And more are coming. The FDA approved 12 new biosimilars in 2024 alone. Experts predict biosimilars could save another $100 billion over the next decade if barriers to use are removed.
Who’s saving the most? It’s not what you think
The biggest savings don’t come from rare drugs. They come from the ones millions of people take every day. The top 10 generic drugs by savings in 2023 accounted for $127 billion-nearly a third of all generic savings. These are drugs for high blood pressure, cholesterol, diabetes, and depression. Think lisinopril, atorvastatin, metformin, sertraline. These aren’t flashy breakthroughs. They’re the foundation of everyday health. And they’re the reason millions of people can afford to stay on their meds.State-level savings vary wildly. California saved nearly $38 billion in 2023. Alaska, with a smaller population, saved $600 million. But even in smaller states, the impact is real. A person on insulin who switches from a $300 brand-name version to a $40 generic doesn’t just save money-they save their life. That’s the real metric.

Why aren’t we saving even more?
The system works-but it’s being sabotaged. Big pharmaceutical companies don’t want to lose their monopoly. So they use tricks to delay generics. One common tactic is “patent thickets”-filing dozens of minor patents on a single drug, just to keep competitors out. A 2024 study found that just four brand-name drugs used this strategy to block generics for years, costing the system over $3.5 billion in lost savings.Another trick is “pay-for-delay.” Brand companies pay generic makers to hold off on launching their cheaper version. The Congressional Budget Office estimates this costs taxpayers $12 billion a year. Then there’s “product hopping”-when a company slightly changes a drug’s form (like switching from a pill to a capsule) and gets a new patent, forcing patients to switch to the more expensive version.
Even when generics are available, insurance plans sometimes don’t make them easy to get. Pharmacy Benefit Managers (PBMs), who negotiate drug prices for insurers, sometimes push patients toward brand-name drugs because they get bigger rebates from manufacturers. A 2023 survey found that 42% of patients skipped doses or didn’t fill prescriptions because of cost. But among those who switched to generics, 89% said they were happy with the results and saved an average of $147 per month.
What’s next? The road ahead
The FDA approved 1,145 new generic drugs in 2024-up 7.3% from the year before. That’s good news. But supply chain problems are a growing threat. As of December 2024, 287 generic medications were in short supply, mostly because manufacturing is concentrated in just a few countries. And the market is getting more concentrated too. The top 10 generic drugmakers now control 63% of the U.S. market, up from 51% in 2015. That reduces competition, which can slow price drops.There’s hope. In June 2024, the Senate HELP Committee passed a bill called the Affordable Prescriptions for Patients Act. It targets patent abuse and pay-for-delay deals. The Congressional Budget Office estimates it could save $7.2 billion a year. If passed, it would be the biggest step toward unlocking the full potential of generics in decades.
Meanwhile, the trend is clear: the more generics used, the more money saved. The IQVIA Institute projects that from 2025 to 2034, generics and biosimilars will save the U.S. healthcare system another $5.1 trillion. That’s not a prediction. It’s a baseline-if we stop letting corporate loopholes get in the way.
Real people, real savings
On Reddit, one user shared: “I was paying $800 a month for my brand-name antidepressant. My pharmacist said, ‘Try the generic.’ I did. Same effect. $10 a month. I cried.” That’s not an outlier. It’s the norm. Thousands of people like them are living longer, healthier lives because they can afford their meds. And it’s not charity. It’s smart economics.Generics don’t just lower prices. They make healthcare possible. Without them, millions would drop off insurance. Hospitals would be overwhelmed. Public programs would collapse. The system isn’t perfect. But the cheapest, most effective part of it-generic drugs-is working better than almost anything else in American medicine.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and extent. Studies show generics are just as safe and effective. In fact, the same companies often make both the brand and generic versions-just under different labels.
Why do some people say generics don’t work as well?
Some patients report differences, but it’s rarely because the medicine doesn’t work. Generic drugs can have different inactive ingredients-like fillers or dyes-which might affect how a pill feels or tastes. For most people, this doesn’t matter. But for those with rare allergies or absorption issues, switching can cause minor side effects. If you feel a difference, talk to your doctor. Don’t assume the generic failed. Often, it’s just your body adjusting.
Why are generics cheaper if they’re the same?
Brand-name companies spend billions developing a drug and marketing it. Once the patent expires, multiple generic manufacturers enter the market and compete on price. That competition drives costs down. Generics don’t need to spend on advertising or recoup R&D. Their cost is mostly manufacturing and distribution. That’s why a $400 brand pill can become a $4 generic.
Can I ask my pharmacist to switch me to a generic?
Yes, in most cases. Pharmacists are allowed to substitute generics unless the doctor writes “Dispense as Written” or “No Substitution.” If your prescription is for a brand-name drug and you’re paying a lot, ask your pharmacist if a generic is available. It’s your right to know. Many pharmacies will automatically switch you unless you say no.
Do insurance plans encourage generics?
Most do. Many insurance plans have lower copays for generics. Some even require you to try a generic before covering the brand-name version. But not all plans are fair. Some PBMs push brand-name drugs because they get kickbacks from manufacturers. If you’re paying more than you should, call your insurer. Ask why the generic isn’t the default option.
What’s the difference between a biosimilar and a generic?
Generics are exact copies of simple chemical drugs. Biosimilars are highly similar to complex biological drugs made from living cells. They’re not identical, but they’re proven to work the same way. Biosimilars are harder to make and more expensive to develop, so they’re not as cheap as traditional generics-but still 15% to 35% cheaper than the original biologic.


Anna Roh
December 11, 2025 AT 05:21Wow, I had no idea generics saved that much. I just thought they were cheaper because they were junk. Guess I was wrong.
Now I feel kinda dumb for always avoiding them.
Richard Eite
December 12, 2025 AT 03:33USA still the only country where this works because we dont have socialist price controls
Other nations pay 10x more for the same pills
Generic drugs prove capitalism saves lives
Katherine Chan
December 12, 2025 AT 20:02This is one of those stories that makes you believe in people again
Not some flashy tech or billionaire invention
Just regular folks choosing a $4 pill over a $400 one and changing the whole system
Keep going everyone
We got this
Philippa Barraclough
December 13, 2025 AT 19:08The economic implications of generic drug adoption are profoundly significant when contextualized within the broader framework of pharmaceutical market dynamics and regulatory evolution. The Hatch-Waxman Act of 1984 fundamentally altered the incentive structure for market entry by creating an abbreviated new drug application pathway, thereby reducing barriers to competition. This structural shift, coupled with the FDA's bioequivalence requirements, has resulted in a dramatic decoupling of therapeutic efficacy from brand-name pricing. The data presented, particularly the 90% prescription penetration rate with only 12% cost contribution, suggests a highly efficient market mechanism. However, the persistence of anti-competitive practices such as patent thickets and pay-for-delay agreements indicates regulatory capture by incumbent firms. The emergence of biosimilars introduces further complexity, as their regulatory pathway remains less standardized than traditional generics, potentially limiting scalability. The concentration of manufacturing in geographically limited regions also poses systemic risk, as evidenced by the 287 active shortages in 2024. A comprehensive policy response must address not only market entry but also supply chain resilience and PBM transparency to fully realize the projected $5.1 trillion in savings.
Tim Tinh
December 13, 2025 AT 23:13my grandma switched to generic blood pressure med last year
saved her $200 a month
she said it tasted weird at first but now she forgets which one she’s on
same effect, way less stress
why are we still making this hard?
Olivia Portier
December 15, 2025 AT 21:44Just wanted to say thank you to everyone who takes the generic
You’re not just saving yourself
You’re saving someone else’s parent
Someone’s kid
Someone’s chance to keep living
Small choices, huge ripple effects
Keep choosing smart
Tiffany Sowby
December 16, 2025 AT 13:53Of course it saved money
Because we’re paying for a system that lets drug companies charge $400 for a pill made of $0.10 chemicals
And now we’re patting ourselves on the back for not being completely robbed?
Pathetic.
Asset Finance Komrade
December 17, 2025 AT 15:37Capitalism optimizes for profit, not health.
Generics are a workaround, not a solution.
The real tragedy isn’t the price-it’s that we’ve normalized needing a loophole to survive.
🫡
Ryan Brady
December 18, 2025 AT 04:43My insurance still makes me pay $30 for the generic
Meanwhile the brand is $200
So I guess I’m paying $30 to ‘save’ $170
Who’s really getting rich here?
😂
Raja Herbal
December 19, 2025 AT 22:02India makes 70% of the world’s generics
And we’re all over here acting like it’s magic
Meanwhile our politicians won’t touch a single trade deal to secure supply
Real smart.
👏
Ruth Witte
December 21, 2025 AT 09:55Just switched my anxiety med to generic yesterday
Same exact pill, $12 instead of $180
I cried for 10 minutes
Then I hugged my cat
Then I told 5 friends to check their prescriptions
THIS IS A WIN
💖
Katherine Rodgers
December 22, 2025 AT 19:33generic = cheaper
but also sometimes made in a factory with 3 workers and a dog
you think your $4 pill is safe?
ever check where it came from?
nah
you just wanna feel good
so you ignore the fact that 40% of the world's meds come from places that don't even have clean water
but hey at least you saved $147
congrats 🙃