Hepatitis C & Bone Health Risk Calculator
Patient Information
Your Risk Assessment
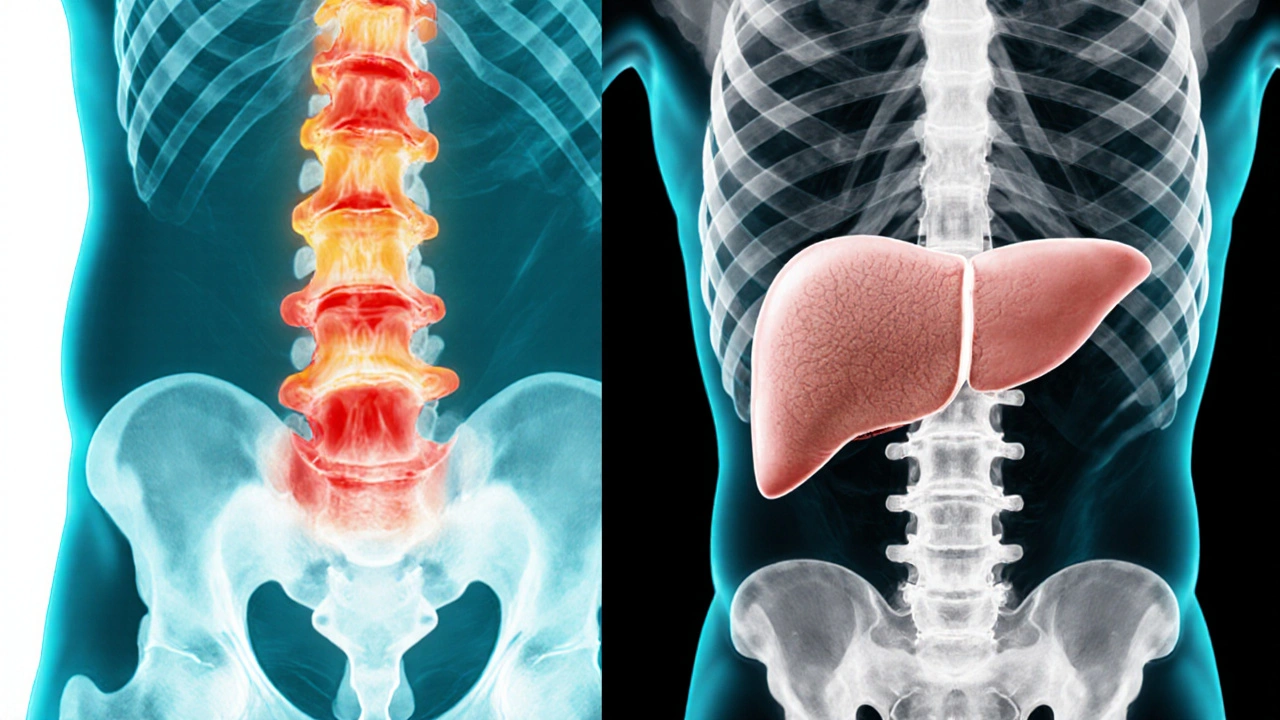
When you hear Hepatitis C and osteoporosis mentioned together, it might sound like a rare coincidence. In reality, chronic Hepatitis C infection quietly speeds up bone loss, putting patients at a higher chance of fractures. This article breaks down why the liver virus matters for your skeleton, how to spot the problem early, and what steps can keep your bones strong.
Key Takeaways
- Chronic Hepatitis C lowers bone mineral density by 5‑12% compared with non‑infected peers.
- Vitamin D deficiency, chronic inflammation, and altered calcium metabolism are the main culprits.
- Screening with a DEXA scan is recommended for all patients over 40 with Hepatitis C.
- Effective antiviral therapy (DAAs) can halt further bone loss, but some patients still need osteoporosis medication.
- Lifestyle measures-adequate Vitamin D, calcium, weight‑bearing exercise-are essential for prevention.
Hepatitis C is a blood‑borne viral infection that primarily damages the liver. Over 71million people worldwide live with chronic Hepatitis C, and if left untreated it can progress to cirrhosis or liver cancer. The disease isn’t confined to the liver; its systemic effects reach the bones, muscles, and immune system.
Osteoporosis is a skeletal disorder characterized by reduced bone mass and micro‑architectural deterioration, leading to an increased risk of fractures, especially in the hip, spine, and wrist. The condition is diagnosed by measuring bone mineral density (BMD) with a dual‑energy X‑ray absorptiometry (DEXA) scan.
Why Hepatitis C Affects Bone Health
The link between Hepatitis C and osteoporosis isn’t a single cause but a web of interrelated factors:
- Chronic inflammation drives the release of cytokines such as IL‑6 and TNF‑α, which stimulate osteoclast activity (the cells that break down bone).
- Patients often develop Vitamin D deficiency due to impaired liver conversion of vitamin D to its active form, reducing calcium absorption. \n
- Progressive liver fibrosis hampers the synthesis of proteins needed for bone matrix formation.
- Many individuals with Hepatitis C have poor nutritional status and lower calcium intake, further weakening bone.
- Alcohol use, a common co‑factor in Hepatitis C, independently contributes to bone loss.
How Much Higher Is the Risk?
Large cohort studies from the United States and Europe consistently show a 30‑45% higher prevalence of osteopenia or osteoporosis in Hepatitis C patients versus age‑matched controls. One meta‑analysis (2023) reported an average BMD reduction of 0.07g/cm² at the lumbar spine-equivalent to moving from a normal T‑score of -0.5 to an osteopenic -1.5.
Screening and Diagnosis
Because bone loss is often silent until a fracture occurs, proactive screening is crucial:
- Who should be screened? All adults with chronic Hepatitis C aged 40+; younger patients with additional risk factors (e.g., long‑term corticosteroid use, heavy alcohol consumption) should also be considered.
- What test? A DEXA scan of the lumbar spine and hip provides the most reliable BMD measurement.
- Interpretation: Use the WHO T‑score categories-normal (≥-1.0), osteopenia (-1.0 to >-2.5), osteoporosis (≤-2.5).
Impact of Antiviral Therapy
Since the arrival of direct‑acting antivirals (DAAs) in 2014, cure rates (sustained virologic response) exceed 95%. These drugs not only halt liver disease progression but also improve bone health:
- Within 12months of a successful DAA regimen, studies show a modest BMD rise of 2‑3%.
- However, patients with advanced fibrosis or cirrhosis may retain residual bone loss and still need osteoporosis treatment.
When counseling patients, emphasize that curing Hepatitis C is a key step toward protecting their bones, but it doesn't replace standard osteoporosis management.
Preventive Lifestyle Measures
Regardless of antiviral status, the following habits cut down fracture risk:
- Vitamin D and calcium: Aim for 800‑1000IU of vitamin D daily and 1200mg of calcium from diet or supplements, after checking serum 25‑OH‑vitamin D levels.
- Weight‑bearing exercise: Activities like brisk walking, resistance training, or dancing for at least 150minutes per week stimulate bone formation.
- Avoid excessive alcohol and smoking: Both accelerate bone resorption and worsen liver disease.
- Monitor liver health: Regular labs and imaging keep fibrosis in check, indirectly supporting bone metabolism.
Managing Osteoporosis in Hepatitis C Patients
If a DEXA scan falls into the osteopenic or osteoporotic range, standard pharmacologic options apply-bisphosphonates, selective estrogen receptor modulators (SERMs), or newer agents like denosumab. The choice should consider liver function:
- Bisphosphonates (alendronate, risedronate) are safe for most patients with compensated liver disease.
- Denosumab is a monoclonal antibody that doesn’t rely on hepatic metabolism and can be used in advanced cirrhosis.
- Regular monitoring of calcium, kidney function, and liver enzymes is essential during therapy.
Comparison of Bone Health Metrics in Hepatitis C vs. General Population
| Group | Mean Lumbar Spine BMD (g/cm²) | Mean Hip BMD (g/cm²) | Prevalence of Osteoporosis |
|---|---|---|---|
| General Population (age45‑65) | 1.02±0.12 | 0.95±0.10 | 8% |
| Chronic HepatitisC (treated) | 0.94±0.11 | 0.88±0.09 | 12% |
| Chronic HepatitisC (untreated) | 0.89±0.13 | 0.82±0.11 | 18% |
Practical Checklist for Patients and Clinicians
- Confirm HepatitisC status and stage of liver disease.
- Order a baseline DEXA scan if age≥40 or earlier with risk factors.
- Check serum 25‑OH‑vitamin D; supplement to reach ≥30ng/mL.
- Prescribe calcium (1,200mg) and vitamin D (800‑1,000IU) if deficient.
- Encourage weight‑bearing exercise at least three times per week.
- Start antiviral therapy with DAAs; document sustained virologic response.
- If BMD ≤-2.5, initiate osteoporosis medication; monitor liver labs every 3‑6months.

Frequently Asked Questions
Does curing Hepatitis C reverse bone loss?
Curing the virus halts further bone loss and can modestly improve BMD, but it rarely restores bone density to pre‑infection levels. Patients with established osteoporosis still need standard treatment.
How often should I get a DEXA scan?
For people with chronic Hepatitis C, a scan every 2‑3years is reasonable if the first result is normal. If osteopenia or osteoporosis is detected, repeat every 12‑18months to gauge treatment response.
Can I take over‑the‑counter calcium supplements safely?
Yes, but stay below 2,000mg per day to avoid kidney stones. Choose a calcium citrate form if you have reduced stomach acid, which is common in liver disease.
Are there any bone‑friendly antiviral regimens?
All modern direct‑acting antivirals (e.g., sofosbuvir‑ledipasvir, glecaprevir‑pibrentasvir) have minimal impact on bone metabolism. Older interferon‑based regimens were linked to higher fracture rates.
What lifestyle changes matter most?
Stopping alcohol, quitting smoking, regular weight‑bearing activity, and maintaining adequate vitamin D and calcium intake are the top three actions that protect both liver and bone health.

Nicole Chabot
October 1, 2025 AT 15:38Hey folks, just wanted to point out that keeping your vitamin D up around 30 ng/mL can really blunt that extra bone‑loss risk you see with Hep C. The calculator even nudges you toward 800‑1000 IU daily, which matches most guidelines. Also, trimming weekly alcohol to under 14 drinks can shave a point off the risk score. If you’re on treatment, the extra two points drop out, so getting cured is a solid move. And don’t forget weight‑bearing exercise – a quick walk or some resistance work three times a week goes a long way.
Sandra Maurais
October 8, 2025 AT 08:46While the article presents a thorough overview, several statements lack proper citation-particularly the claim that untreated Hepatitis C adds three risk points to osteoporosis. 🧐 Moreover, the vitamin D thresholds appear inconsistent with Endocrine Society recommendations. 📚 The checklist is useful, yet the formatting could benefit from clearer hierarchy. 🚫 Lastly, the discussion on bisphosphonates omits potential renal considerations in cirrhotic patients, which is a non‑trivial oversight.
Michelle Adamick
October 15, 2025 AT 01:55Spot on, Sandra! The jargon‑heavy segment on direct‑acting antivirals (DAAs) could definitely be streamlined – those meds are #gamechangers 🚀 for bone health. Also, integrating a quick “🔬Evidence Level” label would make the risk‑score algorithm more transparent. Keep pushing for that tighter evidence base, the community will thank you! 💪
Edward Glasscote
October 21, 2025 AT 19:03Good rundown.
Gaurav Joshi
October 28, 2025 AT 11:11The correlation between Hepatitis C and osteoporosis is often overstated; many studies confound liver fibrosis severity with bone loss, making causality dubious. Additionally, lifestyle factors like smoking and sedentary habits drive the majority of risk, not the virus itself. So, while antivirals help, they aren’t the silver bullet the article hints at.
Jennifer Castaneda
November 4, 2025 AT 04:20There’s a hidden agenda behind the glossy tables and clean graphics you see in these medical write‑ups. Pharma companies have been funneling millions into “bone‑health” research, hoping to open another revenue stream beyond their viral cures. Every time they mention “direct‑acting antivirals” they gloss over the fact that these drugs are patented, pricey, and heavily marketed to patients desperate for a cure. The subtle push to start bisphosphonates or denosumab right after viral eradication is a classic cross‑sell tactic, ensuring they capture both the viral and the skeletal markets. Meanwhile, independent labs that could challenge these narratives are starved of funding, forcing them into the shadows. The data showing a 2‑3% BMD rise after treatment is statistically significant, but clinically, it’s barely enough to offset years of bone loss incurred during chronic infection. The article also drops serum calcium monitoring without emphasizing the risk of hypercalcemia in patients on vitamin D mega‑doses, a loophole that can lead to kidney stones and further complications. They paint a picture of a seamless recovery, yet real‑world adherence to daily supplements is notoriously low, especially in underserved populations. By simplifying the checklist, they mask the complex socio‑economic barriers that prevent patients from actually following through. Moreover, the mention of “weight‑bearing exercise” sounds encouraging, but there’s no discussion of how cirrhosis can limit physical capacity, making the advice unrealistic for many. All these omissions create a narrative that nudges patients toward more pharmaceuticals, which ultimately benefits the bottom line of a few conglomerates. It’s a classic case of medicalization where every symptom becomes a marketable condition. The article’s tone is deceptively neutral, but the underlying message is clear: treat the virus, then treat the bones, and keep the prescription pad busy. Remember, the more you spend on pills, the deeper the financial hook. Stay skeptical, demand raw data, and question why certain recommendations feel more like a sales pitch than genuine care.
Rajan Desai
November 10, 2025 AT 21:28Jennifer raises several pertinent points about funding bias, especially regarding BMD outcomes post‑DAA therapy. While the 2‑3% increase is modest, it is consistently reproduced across randomized cohorts, suggesting a genuine physiological effect rather than mere marketing. Nonetheless, the emphasis on supplement adherence should be paired with community outreach programs to bridge that compliance gap.
Sangeeta Birdi
November 17, 2025 AT 14:36Absolutely, Rajan! 🎯 Engaging local support groups and offering free vitamin D testing can really boost adherence. Let’s keep the conversation focused on practical steps that empower patients. 😊
Chelsea Caterer
November 24, 2025 AT 07:45Its important to check bone densitiy regularly.
Lauren Carlton
December 1, 2025 AT 00:53There are several grammatical inconsistencies throughout the piece, such as the misuse of “its” versus “it’s” in the vitamin D section and the dangling modifier in the sentence about alcohol consumption. Additionally, the bullet points lack parallel structure, alternating between verbs and nouns. These errors detract from the credibility of an otherwise informative article.
Katelyn Johnson
December 7, 2025 AT 18:01Good catch, Lauren. I’ll make sure the next edit aligns the list items and fixes the apostrophe usage. Thanks for keeping the standards high.
Anthony Aspeitia-Orozco
December 14, 2025 AT 11:10The interplay between viral infection and bone metabolism reminds us that health is an intricate web; targeting a single pathogen without addressing systemic factors is akin to treating a symptom while ignoring the root cause. A holistic approach that blends antiviral therapy with lifestyle modification offers the most sustainable path forward.
Adam Dicker
December 21, 2025 AT 04:18Exactly! 🎭 When you knock out Hep C, you’re not just silencing a virus – you’re reclaiming the whole skeletal fortress. Let’s rally behind comprehensive care that hits every weak spot!
Molly Beardall
December 27, 2025 AT 21:26Wow, this article really tries to juggle science and hype, doesn’t it? The clinical data is solid, but the narrative feels like a Hollywood trailer for a blockbuster drug – all flash, little depth. Still, kudos for pulling together the osteoporosis checklist; it’s a lifesaver for clinicians swamped with paperwork. Just wish the authors would tone down the melodrama and stick to the hard facts.
Brian Pellot
January 3, 2026 AT 14:35Heard you, Molly. I think the practical checklist does the heavy lifting, and the rest can be trimmed down for clarity. Happy to see everyone chipping in.