It’s easy to assume that if you have a fever, sore throat, or cough, antibiotics will fix it. But that’s not true-and taking them when you don’t need them can actually make things worse. The difference between a bacterial infection and a viral infection is a fundamental distinction in medicine: bacteria are living cells that can reproduce on their own, while viruses are genetic material wrapped in protein that can only replicate inside human cells. This isn’t just academic-it changes everything about how you’re treated, how long you’ll feel sick, and even whether you risk contributing to a global health crisis.
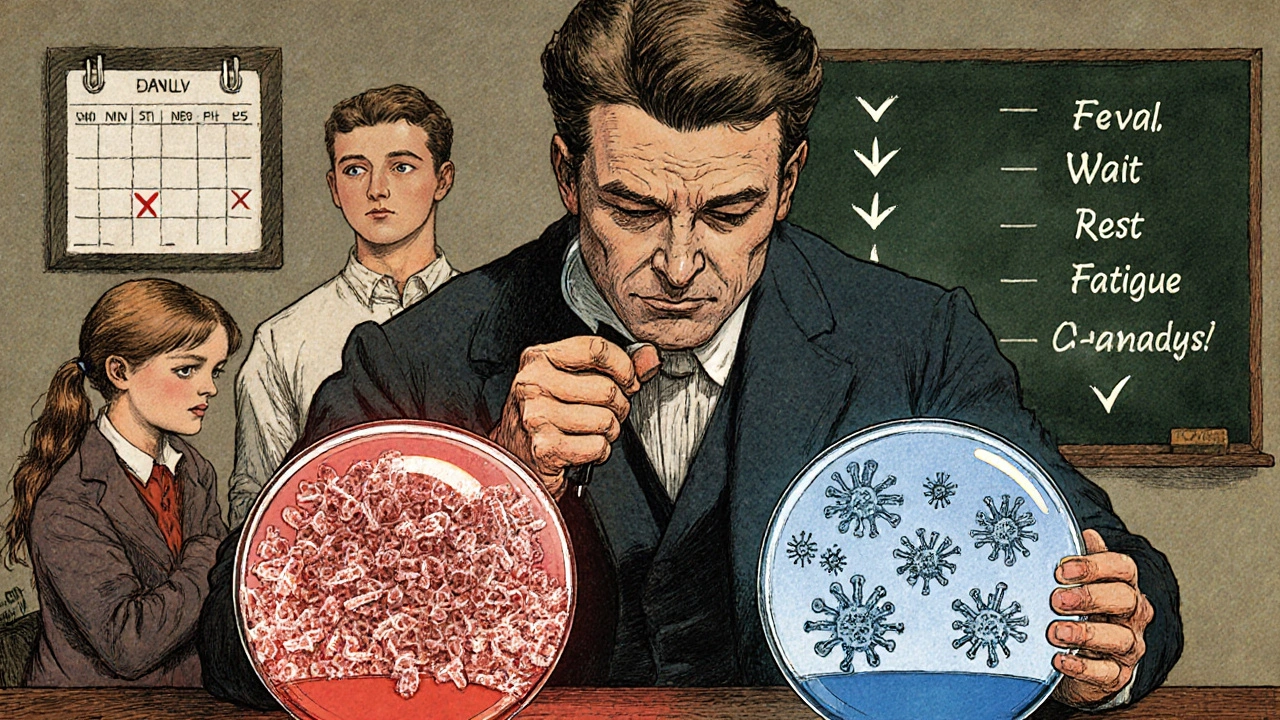
What Exactly Are Bacteria and Viruses?
Bacteria are single-celled organisms. They’re alive, they eat, they grow, and they multiply by splitting in half-sometimes as fast as every 20 minutes. You carry trillions of them on your skin and inside your gut. Most are harmless or even helpful. But some, like Streptococcus pyogenes a bacterium that causes strep throat, can invade your body and cause disease. These infections often show up as localized problems: a red, swollen throat with white patches, a painful urinary tract infection, or a sinus infection with thick yellow-green mucus.
Viruses are completely different. They’re not alive in the way bacteria are. Think of them as tiny genetic codes-either DNA or RNA-packed in a protein shell. They can’t do anything on their own. To multiply, they have to break into your cells and hijack their machinery. Once inside, they force your cells to make copies of the virus until they burst, spreading to other cells. That’s how the influenza virus causes seasonal flu or SARS-CoV-2 triggers COVID-19. Viral infections tend to hit harder and faster: sudden fever, body aches, fatigue, runny nose, and cough.
How Do Symptoms Differ?
Symptoms overlap a lot. Both can cause fever, sore throat, and fatigue. But there are patterns that help doctors tell them apart.
Bacterial infections often come with:
- High fever-above 101°F (38.3°C)
- Symptoms that last longer than 10-14 days
- Worsening after initial improvement (like feeling better for a few days, then crashing again)
- Localized signs: pus, thick colored mucus, or swelling in one area
Viral infections usually show:
- Milder fever-under 100.4°F (38°C)
- Runny nose, sneezing, hoarse voice
- Generalized body aches and tiredness
- Improvement within 7-10 days
But here’s the catch: you can’t always tell just by symptoms. That’s why doctors use tests. A rapid strep test for group A strep the bacterium behind strep throat gives results in minutes and is 95% accurate. For viruses like flu or COVID-19, PCR tests detect genetic material and are 90-95% reliable if done early.
Why Antibiotics Don’t Work on Viruses
Antibiotics are designed to kill bacteria or stop them from multiplying. They target things viruses don’t have: cell walls, protein-making machines, or DNA replication tools. Penicillin works by breaking down bacterial cell walls. Macrolides like azithromycin block bacterial protein production. Viruses don’t have any of these structures. So antibiotics are useless against them.
Yet, in the U.S., doctors prescribe antibiotics for viral infections about 47 million times a year-mostly for colds, flu, and bronchitis. That’s not just a waste of pills. It’s fueling a crisis. Every time you take an antibiotic unnecessarily, you’re giving bacteria a chance to adapt. They evolve. They become resistant. That’s how drug-resistant superbugs like MRSA and multidrug-resistant tuberculosis spread.
The CDC says antibiotic-resistant infections kill 35,900 people in the U.S. every year. Globally, the WHO estimates 1.27 million deaths in 2019 were directly linked to antibiotic resistance. If we keep this up, by 2050, resistant infections could kill 10 million people annually-more than cancer.
What Actually Treats Viral Infections?
For most viral infections, there’s no magic pill. Your immune system does the heavy lifting. Treatment is about support:
- Rest
- Hydration
- Over-the-counter pain relievers like acetaminophen or ibuprofen
- Saline nasal sprays for congestion
There are exceptions. Oseltamivir (Tamiflu) an antiviral for influenza can shorten flu symptoms by 1-2 days if taken within 48 hours of the first sign. Remdesivir used for severe COVID-19 helps hospitalized patients recover faster. Acyclovir treats chickenpox and shingles, both caused by the varicella-zoster virus.
But these are targeted, time-sensitive, and only used in specific cases. Most colds, flu, and bronchitis? No antiviral will help. And giving one anyway does nothing but add cost and side effects.
When Do You Really Need Antibiotics?
Antibiotics are lifesavers when you have a true bacterial infection. But not every infection needs them. Here’s when they’re actually required:
- Confirmed strep throat (via rapid test or culture)
- Bacterial pneumonia (not viral)
- Urinary tract infections (UTIs)
- Some sinus infections-only if symptoms last over 10 days or worsen after improvement
- Skin infections like cellulitis
Doctors use tools like the Centor Criteria to decide if strep is likely. It checks for:
- Tonsil white patches (1 point)
- Tender neck glands (1 point)
- Fever above 100.4°F (1 point)
- No cough (1 point)
If you score 3 or more, there’s a 50-55% chance it’s bacterial-and testing is recommended. If you score 0-1, it’s almost certainly viral. No test needed.

The Bigger Picture: Why This Matters
Every time you take an antibiotic for a cold, you’re not just risking side effects like diarrhea or yeast infections. You’re helping create superbugs. And those superbugs don’t just hurt you-they hurt everyone.
Think about this: 85% of acute bronchitis cases are viral. Yet, in the U.S., doctors still prescribe antibiotics for them 70% of the time. Parents push for antibiotics for their kids’ coughs, not realizing that 70% of childhood sinus infections are viral too. That’s why kids get six to eight colds a year-and parents lose 20 million workdays annually just dealing with them.
And it’s not just about resistance. Antibiotics can trigger deadly infections like Clostridioides difficile a gut bacteria that thrives when normal flora is wiped out by antibiotics. In the U.S., C. diff causes 223,900 infections and 12,800 deaths every year.
The economic cost? $1.1 billion a year in unnecessary antibiotic prescriptions. Viral illnesses cost the U.S. $45 billion in medical bills and lost productivity.
What’s Changing in 2025?
There’s new hope. In 2020, the FDA approved a rapid test called FebriDx a point-of-care test that measures two biomarkers to distinguish bacterial from viral infections. It gives results in 10 minutes with 94% accuracy. Primary care clinics are starting to use it to cut down on wrong prescriptions.
Scientists are also exploring alternatives to antibiotics. Phage therapy using viruses that infect only bacteria has shown 85% success in treating resistant infections in European trials. Researchers at the University of Queensland are testing two new compounds, IMB-001 and IMB-002, that target bacterial surface proteins-potentially bypassing resistance mechanisms.
And there’s progress on vaccines. Universal coronavirus vaccines are in Phase III trials. If they work, they could prevent future pandemics before they start.
What Should You Do If You’re Sick?
Don’t rush to the doctor for antibiotics. Here’s a simple guide:
- Feel sick for less than 7 days? Likely viral. Rest, hydrate, use OTC meds.
- Fever above 101°F, sore throat with white patches, symptoms lasting over 10 days? See a doctor. Ask for a strep test.
- Worsening after feeling better? Could be a secondary bacterial infection. Get checked.
- Don’t pressure your doctor for antibiotics. Say: "Is this bacterial or viral? Can we test for it?"
It’s hard to watch your child suffer or feel awful yourself. But the right treatment isn’t always the fastest one. Sometimes, waiting is the smartest thing you can do.
Can a viral infection turn into a bacterial one?
Yes. A viral infection like the flu or a cold can weaken your airways, making it easier for bacteria to invade. This is called a secondary infection. For example, about half of hospitalized patients with severe viral pneumonia develop a bacterial lung infection. That’s why doctors sometimes prescribe antibiotics after a viral illness-if symptoms suddenly worsen after a few days of improvement.
Do I need antibiotics for a sinus infection?
Not usually. About 90% of sinus infections are viral and clear up on their own in 7-10 days. Antibiotics are only needed if symptoms last longer than 10 days, get worse after improving, or involve high fever and thick colored mucus. Even then, doctors often wait a few days to see if it clears on its own before prescribing.
Why do doctors sometimes prescribe antibiotics for viral infections?
Sometimes, it’s pressure from patients who expect a prescription. Other times, doctors are unsure and take the "safe" route. But research shows that when patients understand the difference, they’re happy to wait. A 2022 JAMA study found that patients who got antibiotics for viral infections were 65% more likely to return for the same symptoms later-because they learned to expect a pill, not rest.
Can I take antivirals for the common cold?
No. There are no approved antivirals for the common cold, which is usually caused by rhinoviruses. Antivirals like Tamiflu only work for specific viruses like influenza or herpes-family viruses. For colds, rest and fluids are the only proven treatments.
How long does it take to recover from a viral infection?
Most viral infections like colds or flu improve within 7-10 days. Fatigue and cough can linger for a couple more weeks, but that’s normal. If you’re not feeling better after 10 days, or you start getting worse, it could be a bacterial complication-and you should see a doctor.
If you’ve ever been told, "Take these antibiotics, you’ll feel better tomorrow," and didn’t-you’re not alone. The truth is, healing takes time. And sometimes, the most powerful medicine is patience.

Andy Slack
November 9, 2025 AT 16:40Finally someone explains this without the medical jargon overload. I used to beg my doctor for antibiotics every time I had a cold. Now I just drink tea, sleep, and wait. My immune system isn’t lazy-it’s just doing its job.
Rashmi Mohapatra
November 9, 2025 AT 20:18bro why u even go to doc for cold? u get flu? rest. u get cough? honey n lemon. antibiotics? nope. my aunt in delhi used to say 'bacteriya ke liye pill, virus ke liye time' and she was right lol
Abigail Chrisma
November 9, 2025 AT 23:53This is such an important conversation to have. I work in pediatric nursing and I see parents panic when their kid has a fever for three days. We spend so much time educating them that it’s not always about killing something-it’s about giving the body space to heal. Thank you for sharing this clearly.
Also, the part about C. diff? That’s terrifying and under-discussed. I’ve seen kids get it after just one round of amoxicillin for an ear infection that was probably viral. It’s not just about resistance-it’s about collateral damage to our microbiomes.
And yes, the FebriDx test? We started using it last year. Game changer. Parents are way more okay with waiting when they see a number that says ‘viral’ instead of just being told ‘it’s probably nothing’.
Ankit Yadav
November 10, 2025 AT 03:36Doctors prescribe antibiotics because they’re tired of being yelled at for not giving them. Patients want a pill. They don’t want to hear ‘wait and see.’ It’s a system problem not a doctor problem. We need better public education and faster diagnostics. Until then, we’re stuck playing whack-a-mole with superbugs
Meghan Rose
November 10, 2025 AT 09:13Okay but what if you’re the person who gets pneumonia every time you get a cold? And your doctor says ‘wait’ and then you end up in the hospital? So now you’re supposed to just trust that your body will magically fix it? What if it doesn’t? What if you’re one of the 5% who actually do need antibiotics early? You’re just supposed to gamble with your life because some blog says ‘rest and hydrate’?
Also why is everyone so sure about this? I’ve had viral infections that turned into bacterial ones in 48 hours. You don’t get to play doctor with people’s health.
Steve Phillips
November 11, 2025 AT 12:07Oh, wonderful. Another sanctimonious, pseudo-scientific manifesto disguised as public health advice. Let me guess-you also think fluoride is a government plot and that vitamin C cures cancer? This article reads like it was written by a med student who just finished their first microbiology lecture and now thinks they’re Dr. Fauci’s heir apparent.
Antibiotics? ‘Waste of pills’? HA! Have you ever had a ruptured appendix? A necrotizing fasciitis? A septic joint? No? Then shut up. The fact that you think ‘rest and hydration’ is a substitute for modern medicine is not just naive-it’s dangerously arrogant. And don’t get me started on ‘phage therapy.’ That’s not a cure-it’s a footnote in a 1940s Soviet journal.
Also, the CDC stats? Misleading. They conflate hospital-acquired infections with community ones. And the ‘10 million deaths by 2050’? That’s a projection based on assumptions that assume we won’t innovate. Which we will. Because humans always do. Unlike you, who thinks the answer is to sit on your hands and pray to the God of Natural Immunity.
Rachel Puno
November 12, 2025 AT 11:56I love how this breaks it down without shaming anyone. I used to be the mom who demanded antibiotics for my kid’s cough. Then I read about how it was making him more prone to ear infections. Now I ask ‘Is this bacterial?’ and wait. It’s hard. But it’s worth it.
Also-thank you for mentioning the Centor Criteria. That’s not common knowledge. If more people knew that no cough + white patches = higher chance of strep, we’d cut down on so many unnecessary tests.
Rest isn’t laziness. It’s medicine.
Clyde Verdin Jr
November 13, 2025 AT 12:16So let me get this straight-you’re saying I should suffer through a week of coughing because some guy in a lab coat says ‘viruses are just genetic code in a protein shell’? That’s not science, that’s a TED Talk script. Meanwhile, my neighbor took amoxicillin for his ‘cold’ and now he’s fine. I’m fine too. Coincidence? I think not.
Also, phage therapy? Sounds like something from a sci-fi movie. And ‘universal coronavirus vaccines’? Yeah right. Next you’ll tell me we’re all going to live to 150 because we drank kombucha.
Bottom line: if I feel like crap, I want a pill. Not a lecture. And if your ‘natural healing’ makes me miss work, you’re the problem.
Key Davis
November 14, 2025 AT 14:08It is with profound respect for the scientific method and the public health imperative that I acknowledge the clarity and rigor of this exposition. The distinction between bacterial and viral etiologies is not merely academic; it is foundational to evidence-based clinical decision-making. The unintended consequences of antimicrobial overuse-particularly the emergence of multidrug-resistant organisms-constitute a global biosecurity threat of the highest order.
Furthermore, the integration of point-of-care diagnostics such as FebriDx represents a paradigm shift toward precision medicine in primary care. One must also recognize the cultural and psychological dimensions of patient expectations, which often conflict with clinical best practices. This requires not only education, but also structural reforms in healthcare delivery.
It is my sincere hope that this message reaches not only clinicians, but also policymakers, educators, and the general public.
Cris Ceceris
November 15, 2025 AT 16:27I’ve been thinking about this a lot lately. We treat illness like it’s a bug to be fixed, not a signal from our bodies. Bacteria and viruses aren’t enemies-they’re part of the ecosystem we live in. The real problem isn’t the infection-it’s how disconnected we’ve become from our own biology.
Why do we expect instant fixes? Why do we think medicine should always be a pill? Maybe the real cure is learning to listen-to rest, to slow down, to trust our bodies more. Antibiotics are powerful, yes. But so is patience.
And maybe that’s the hardest medicine of all.
Brad Seymour
November 16, 2025 AT 02:37Love this. As someone from the UK, I’ve seen the NHS push back hard on antibiotic prescribing-and it’s working. We used to have a culture of ‘doctor, give me something for this cough’ and now? People say ‘is it viral?’ and nod when they hear yes. It’s a quiet revolution.
Also, the bit about C. diff? Yeah, that’s real. My mum got it after a course of clindamycin for a tooth infection. She was in the hospital for weeks. No one told her that antibiotics could do that. We need more of this info out there.
Malia Blom
November 16, 2025 AT 14:47Wow, what a load of oversimplified nonsense. You act like viral infections are harmless and bacterial ones are the villains. But what about chronic viral infections? Like Epstein-Barr triggering autoimmune disease? Or HPV causing cancer? Or herpes reactivating during stress? Viruses are way more dangerous than you’re letting on.
And let’s not forget-antibiotics aren’t the only problem. The pharmaceutical industry profits from both antibiotics AND antivirals. So who’s really benefiting from this ‘don’t take antibiotics’ narrative? Maybe the same people who sell you probiotics and essential oils.
This isn’t science. It’s marketing.
Erika Puhan
November 18, 2025 AT 08:44Let’s be clear: the overprescription of antibiotics is a direct result of Western medical incompetence. In India, we’ve always known that fever + cough = viral. You take neem, turmeric, and rest. No pills. No panic. But Americans? They want a pill for everything-even existential dread. And now they’re paying the price with superbugs. This is what happens when you outsource health to Big Pharma.
Also, phage therapy? We’ve been using it since the 1920s in Georgia. You just didn’t know because it wasn’t patented.
Edward Weaver
November 19, 2025 AT 05:32Antibiotics are a gift from God to American ingenuity. You think those superbugs are bad? Try living in a country where people don’t even have access to penicillin. We don’t need to be guilt-tripped for saving lives. We need to keep making pills that work. If you don’t like it, move to a country where they still use leeches.
And don’t get me started on ‘rest and hydration.’ That’s what you tell people who can’t afford to miss work. Meanwhile, I’ve got a family to feed and a job that doesn’t care if I’m coughing up a lung.
This isn’t about science. It’s about privilege.