When your thyroid goes off track, your whole body feels it. You might be tired all the time, gain weight without eating more, or feel cold even in summer. Or maybe you’re losing weight despite eating like a horse, your heart races for no reason, and you can’t sit still. These aren’t just quirks of aging or stress-they could be signs of a thyroid problem. Hypothyroidism and hyperthyroidism are two sides of the same coin: one means your thyroid is too slow, the other too fast. Both are common, often misunderstood, and easy to miss-until you start connecting the dots.
What’s Actually Happening in Your Body?
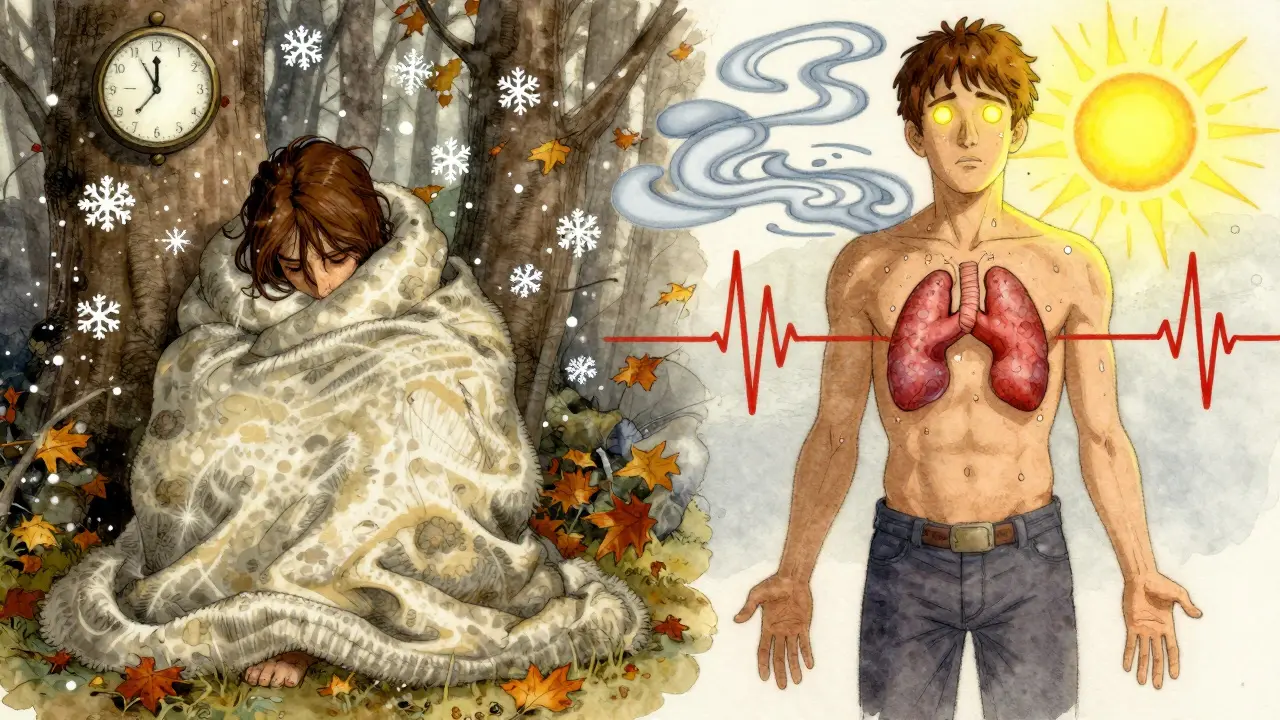
Your thyroid is a small butterfly-shaped gland at the base of your neck. It doesn’t make much hormone, but what it does make controls how every cell in your body uses energy. It’s like the thermostat for your metabolism. When it’s working right, you feel steady-energized but not wired, warm but not sweaty, regular but not bloated. In hypothyroidism, your thyroid doesn’t make enough T4 and T3 hormones. Your body slows down. In hyperthyroidism, it makes too much. Your body speeds up. It’s not just about feeling tired or anxious-it’s about measurable changes in your heart rate, body temperature, digestion, and even your menstrual cycle. The most common cause of hypothyroidism is Hashimoto’s thyroiditis, an autoimmune condition where your immune system attacks your thyroid. For hyperthyroidism, it’s usually Graves’ disease-another autoimmune issue, but this time your immune system overstimulates the gland. Both are more common in women, especially after 50. In fact, women are five to eight times more likely to develop thyroid problems than men.Symptoms: Slow Down vs. Speed Up
The symptoms of these two conditions look almost like opposites-and that’s the key to spotting them. If you have hypothyroidism, you might notice:- Constant fatigue-even after a full night’s sleep
- Weight gain of 10 to 30 pounds without changes in diet or activity
- Feeling cold when others are fine
- Dry skin, brittle hair, or hair loss
- Constipation
- Depression or brain fog-like you’re thinking through fog
- Heavier or irregular periods
- Heart rate below 60 beats per minute
- Unexplained weight loss, even with increased hunger
- Feeling hot, sweating more than usual
- Rapid heartbeat-often over 100 bpm, sometimes over 140
- Tremors in your hands
- Anxiety, panic attacks, or feeling on edge
- Frequent bowel movements or diarrhea
- Lighter or missed periods
- Swelling in the neck (goiter), and sometimes bulging eyes if it’s Graves’ disease
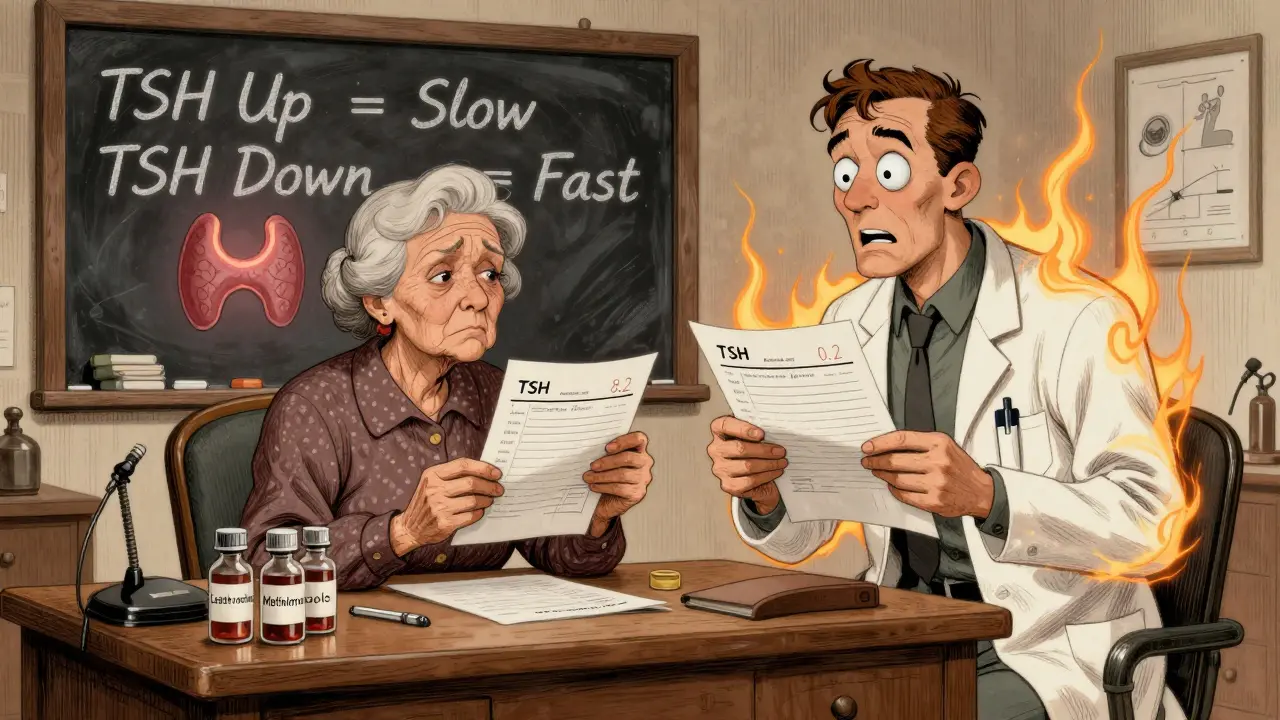
How Doctors Diagnose It
You can’t diagnose this yourself by symptoms alone. That’s why blood tests are non-negotiable. The first test is always TSH-thyroid-stimulating hormone. It’s made by your pituitary gland and tells your thyroid when to produce more hormones. If your thyroid is underactive, your pituitary yells louder-so TSH goes up. If your thyroid is overactive, your pituitary shuts up-so TSH drops.- Hypothyroidism: TSH above 4.5 mIU/L, free T4 below normal
- Hyperthyroidism: TSH below 0.4 mIU/L, free T4 and/or T3 above normal
Treatment: One Pill vs. Multiple Paths
Hypothyroidism treatment is simple: take a daily pill called levothyroxine. It replaces the T4 your body isn’t making. Most people start at 1.6 mcg per kilogram of body weight. It takes 6 to 8 weeks to feel the full effect. Your doctor will check your TSH every 6 to 8 weeks until it’s stable, then usually once a year after that. But here’s the real-world problem: 45% of people don’t take it right. Levothyroxine must be taken on an empty stomach, 30 to 60 minutes before breakfast. Coffee, calcium, iron, and even soy can block absorption. If you take it with your morning vitamins or your oatmeal, it won’t work. One study found that patients who got clear instructions on timing had 35% better adherence and fewer ER visits. Hyperthyroidism? It’s messier. First-line treatment is usually methimazole, a pill that blocks hormone production. Doses range from 5 to 60 mg a day. You’ll need monthly blood tests to watch for rare but serious side effects like liver damage or low white blood cells. Another option is radioactive iodine. You swallow a capsule, and the radiation destroys overactive thyroid cells. It’s effective-but in 80% of cases, it leads to hypothyroidism. That means you’ll spend the rest of your life taking levothyroxine anyway. Thyroid surgery is less common but used if the gland is huge, if there are nodules, or if you can’t take meds. It’s permanent-you’ll need lifelong thyroid hormone replacement. Pregnant women face special challenges. Propylthiouracil is sometimes used in early pregnancy, but it carries a 1 in 5,000 risk of severe liver injury. That’s why doctors try to switch to methimazole after the first trimester.Why Some People Still Don’t Feel Right
Here’s where things get personal. Many people take their levothyroxine, get their TSH back to normal, and still feel awful. Brain fog. Exhaustion. Weight that won’t budge. Their doctor says, “Your labs are perfect.” But they’re not. About 15% of people have genetic differences in the enzymes that convert T4 to T3-the active form of thyroid hormone. If your body can’t make enough T3, even perfect TSH levels won’t fix how you feel. Some doctors now test for free T3 or consider adding a small amount of T3 (liothyronine) to the regimen. It’s not standard yet, but it’s becoming more common. On patient forums, you’ll hear stories like: “I take 100 mcg of levothyroxine daily. My TSH is 2.1. My doctor says I’m fine. But I still can’t remember names. I’m exhausted. I feel broken.” That’s not in your head. It’s real-and it’s more common than you think.
Who’s at Risk?
Women over 50 are the highest-risk group. One in 10 women in that age range has hypothyroidism. But it’s not just age. Other risk factors include:- Family history of thyroid or autoimmune disease
- Previous thyroid surgery or radiation
- Having another autoimmune condition like type 1 diabetes or rheumatoid arthritis
- Being postpartum (thyroid issues often show up 6 to 12 months after giving birth)
- Living in an area with low iodine intake (rare in Australia, but still relevant in some regions)
What’s New in 2026?
Research is moving fast. In 2023, the FDA approved a new drug called resmetirom for a rare condition called thyroid hormone resistance. While it’s not for regular hypothyroidism or hyperthyroidism, it’s part of a bigger trend: personalized thyroid care. Doctors are starting to look beyond TSH. Genetic testing for deiodinase enzyme variations is becoming more accessible. AI tools are helping spot patterns in symptoms and lab results faster. And the American Thyroid Association now recommends earlier use of radioactive iodine-even in younger patients-because it’s more definitive and reduces long-term complications. The big takeaway? Thyroid disorders aren’t just about hormone levels. They’re about how your body responds to those levels. And treatment isn’t one-size-fits-all.What to Do Next
If you’ve been feeling off for months-tired, gaining weight, anxious, or just not yourself-ask your doctor for a TSH test. Don’t wait for a full checklist of symptoms. You don’t need to feel extreme to have a problem. If you’re already diagnosed:- Take your levothyroxine on an empty stomach, 30 minutes before food or coffee
- Don’t skip your blood tests-even if you feel fine
- Track your symptoms, not just your labs
- Ask about free T3 if you’re still struggling
- Know your options if you have hyperthyroidism: meds, ablation, or surgery

Ken Porter
January 7, 2026 AT 18:51Finally, someone breaks it down right. No fluff, just facts. TSH above 4.5? Time to act. Too many docs wait till you’re falling apart.
Molly Silvernale
January 9, 2026 AT 00:36Thyroid isn’t a switch-it’s a symphony. And most doctors are conductors who only know one instrument. I’ve been on levothyroxine for seven years. My TSH is ‘perfect’… but my brain? Still foggy. I swear, if I had a dollar for every time a doctor said ‘your labs are fine,’ I’d own a yacht. But I don’t. Because my T3 is trash. And no one checks it. Why? Because it’s ‘not standard.’
Standard is what they teach in med school. Reality? We’re all different. My body doesn’t convert T4 like yours. My mitochondria are lazy. My enzymes? Broken. And yet-I’m told I’m fine. Just take the pill. Sleep it off. Maybe you’re just depressed.
Depressed? I’m not. I’m just… exhausted. Like my cells forgot how to breathe. I’ve tried everything: selenium, zinc, desiccated thyroid, even raw thyroid gland supplements (yes, really). Nothing worked until I added liothyronine. Now? I can remember my kids’ names. I can walk up stairs without gasping. I’m not cured. I’m just… alive again.
So if you’re reading this and you feel broken? You’re not. You’re just misunderstood. Ask for free T3. Push back. Your body isn’t broken-it’s just ignored.
Manish Kumar
January 9, 2026 AT 17:14Actually, you know what’s funny? In India, we don’t even have access to T3 testing. Most people get TSH and that’s it. And if your TSH is ‘normal,’ you’re told to eat more curry and stop being lazy. I had a cousin who lost 20 kilos in three months, was sweating through her saris, and her doctor told her it was ‘stress from marriage.’ She ended up in the ER with atrial fibrillation. No one even thought of thyroid. We need more awareness here. Not just in the West.
Also, I read somewhere that 70% of Indian women over 45 have subclinical hypothyroidism, but they never get tested because they think it’s just ‘menopause.’ It’s not. It’s autoimmune. And it’s silent. And it kills slowly.
And let’s not forget the iodine thing. We use iodized salt, sure, but in rural areas? Many don’t. And then there’s soy-so much soy in our diets now. Tofu, soy milk, soy sauce. It blocks absorption. So you take your pill, eat your tofu, and wonder why nothing changes. It’s not your fault. It’s the system.
Donny Airlangga
January 10, 2026 AT 22:23I just want to say thank you for writing this. My mom was misdiagnosed for five years. She was told she was ‘just getting old.’ She stopped cooking, stopped talking, stopped caring. We thought it was dementia. Then her sister had the same symptoms-and got tested. TSH was 18. She started levothyroxine. Within three weeks, she was making her famous curry again. She cried. I cried. It wasn’t just hormones. It was her soul coming back.
So if you’re reading this and you’re scared to ask your doctor for a test? Do it. Even if you only have three symptoms. Even if you think it’s ‘in your head.’ It’s not. And you deserve to feel like yourself again.
Lois Li
January 11, 2026 AT 19:34Thank you for mentioning the 60% undiagnosed stat. I’m one of them. I thought I was just lazy. Turns out I had Hashimoto’s for eight years. I gained 50 pounds. I cried for no reason. I forgot my own phone number once. I thought I was losing my mind. Then I found a functional medicine doctor who checked free T3, reverse T3, and thyroid antibodies. My TSH was 8.7. My antibodies were through the roof. I started on levothyroxine. And then I stopped eating gluten. And then I started taking selenium. And slowly, I got my life back.
It’s not magic. It’s science. But it takes patience. And you have to be your own advocate. Your doctor won’t always know. But you can learn. And you can heal.
christy lianto
January 13, 2026 AT 18:48Stop normalizing fatigue. Stop telling women they’re just ‘stressed.’ You’re not tired because you’re busy-you’re tired because your thyroid is dying. And if your doctor won’t listen, find another one. Your life is not a suggestion.
swati Thounaojam
January 14, 2026 AT 12:31My aunt had this. She was always cold. Always tired. We thought she was just old. Then she collapsed. Turned out her TSH was 32. She’s on meds now. She’s alive. Thank you for sharing this.
Annette Robinson
January 14, 2026 AT 22:55Levothyroxine timing matters more than most people realize. I used to take mine with my coffee and vitamins. My TSH stayed high. I switched to taking it with water, 45 minutes before breakfast. Three months later, my energy came back. It’s not a miracle drug-it’s a precision tool. Treat it like one.
Prakash Sharma
January 16, 2026 AT 22:22Why are we letting Big Pharma dictate thyroid treatment? Radioactive iodine? That’s not treatment-that’s surrender. They want you dependent on pills for life. Why not try natural iodine, selenium, and acupuncture? I’ve seen people reverse Graves’ with diet alone. Why is no one talking about this?
Kristina Felixita
January 17, 2026 AT 00:25My sister had Graves’ and went blind from the bulging eyes. She got radioactive iodine. Now she’s hypothyroid. She’s on levothyroxine. She’s fine. But she’ll never get her vision back. This isn’t just about labs. It’s about your eyes. Your heart. Your future. Please don’t wait. Get tested.
Joanna Brancewicz
January 17, 2026 AT 15:47Free T3 is critical. Deiodinase polymorphisms are underdiagnosed. TSH normalization ≠ clinical resolution. Evidence-based practice must evolve beyond TSH-centric paradigms.
Evan Smith
January 17, 2026 AT 21:58So… you’re telling me I’ve been taking my thyroid pill with my oatmeal and coffee for five years… and that’s why I still feel like a zombie? Wow. I’m dumb. But also… thanks. I’m changing my routine tomorrow.
Luke Crump
January 19, 2026 AT 02:52Everyone’s acting like this is some groundbreaking revelation. Newsflash: thyroid disease has been around since 1800. We’ve known about TSH since 1956. The real problem? Medicine still treats symptoms instead of causes. And the real cause? Chronic inflammation. Environmental toxins. Gut dysbiosis. Stress. But nope-just take a pill. That’s the American way. Profit over cure.
And don’t even get me started on ‘resmetirom.’ Another expensive drug for a system that’s broken. We’re not fixing the root. We’re just slapping on more bandages.
Aubrey Mallory
January 19, 2026 AT 03:07I’m a nurse. I’ve seen too many women dismissed. ‘It’s just anxiety.’ ‘You’re perimenopausal.’ ‘Just lose weight.’ I had a patient who came in with a TSH of 24. She’d been told she was ‘just depressed’ for two years. She cried when she got her diagnosis. She said, ‘I thought I was broken.’ We’re not broken. We’re misdiagnosed.
If you’re reading this and you’re a woman over 40? Get tested. No excuses. Your body is trying to tell you something. Listen.
Dave Old-Wolf
January 19, 2026 AT 17:53My dad had apathetic thyrotoxicosis. He was 72. We thought he had Alzheimer’s. He stopped recognizing us. Didn’t eat. Just sat. Then his primary care doc ordered a TSH. It was 0.02. He had Graves’. Radioactive iodine. Now he’s on levothyroxine. He’s back. But we lost a year. Please, if someone you love is acting ‘off’ and it’s not depression-check the thyroid.