- 10
Drug Dosing Adjustment Calculator
This calculator helps you understand how your age, kidney function, and liver function affect drug dosing requirements. Results are estimates and should not replace medical advice.
Your Information
Drug Information
Adjusted Dose Recommendation
Enter your information to see dose adjustments
How This Works
This calculator estimates how your kidney function (based on creatinine levels) and liver function affect drug dosing. For example:
- Vancomycin: Kidney function directly affects clearance rate
- Warfarin: Liver function impacts metabolism
- Age: Older patients often need lower doses
Ever wonder why that pill you took at 8 a.m. makes you drowsy by noon, or why your grandma gets sick from a dose that works fine for you? It’s not magic. It’s pharmacokinetics-the science of how your body handles drugs. This isn’t just textbook stuff. It’s the reason some people have bad reactions to medications while others don’t. Understanding this process can help you avoid dangerous side effects, make better decisions with your prescriptions, and even explain why your doctor keeps adjusting your dose.
What Happens When You Take a Pill?
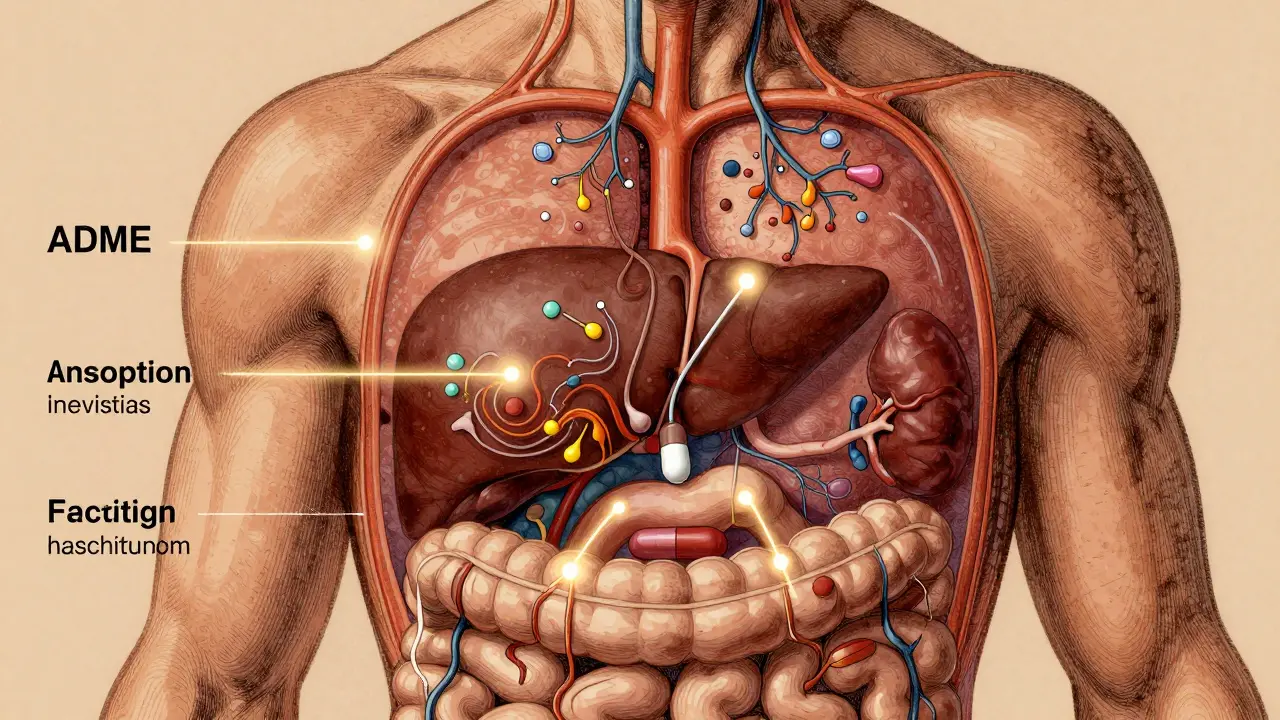
When you swallow a tablet, inject a shot, or apply a patch, your body doesn’t just accept the drug and call it a day. It goes through four key steps: Absorption, Distribution, Metabolism, and Excretion. Experts call this the ADME process, and it’s been the backbone of drug safety since the 1970s. Each step controls how much of the drug actually reaches your target-and how long it sticks around.Let’s say you take an oral painkiller. First, it has to get absorbed through your stomach or intestines. Not all drugs do this equally. Some are broken down by stomach acid before they even leave your gut. Others get blocked by a protein called P-glycoprotein, which acts like a bouncer at the door of your cells. If you’re on a drug like digoxin, this bouncer can cut absorption by up to 70%. That’s why some people just don’t feel the effect-even when they take the right dose.
Why Your Body Might Not Handle Drugs Like Someone Else’s
Once the drug gets into your bloodstream, it starts circulating. But here’s the catch: not all of it is free to work. Many drugs, like warfarin (a blood thinner), bind tightly to proteins in your blood. In fact, 98% of warfarin is stuck to proteins, leaving only 2% active. If you have low protein levels due to illness or malnutrition, more of the drug becomes free-and that can push you into overdose territory without changing your dose.Then comes metabolism. Most drugs are processed in the liver by a family of enzymes called Cytochrome P450. One enzyme, CYP3A4, handles about half of all medications you’ll ever take. But here’s the kicker: your genes determine how fast this enzyme works. About 3-10% of white people have a slow version of CYP2D6, which means they can’t turn codeine into its active form. For them, the painkiller doesn’t work. But for others, it turns into too much morphine too fast, causing dangerous breathing problems.
Age plays a huge role too. By the time you hit 65, your liver processes drugs 30-50% slower than it did in your 20s. Your kidneys, which clear drugs from your body, also lose 30-40% of their function. That’s why older adults are three times more likely to end up in the ER because of side effects. A dose that’s perfect for a 40-year-old could be toxic for a 75-year-old.
How Drug Interactions Turn Safe Meds Into Danger Zones
Many people don’t realize that what you take with your meds matters just as much as the meds themselves. Take statins, for example. They’re used to lower cholesterol. But if you take them with clarithromycin (an antibiotic), your body can’t break down the statin properly. Levels of the statin can spike by 10 times. That might sound harmless, but it raises your risk of rhabdomyolysis-a condition where muscle tissue breaks down and can wreck your kidneys. The risk jumps from 0.04% to 0.5%. That’s not rare. It’s predictable.Even grapefruit juice can mess with this. It blocks the same liver enzyme that breaks down dozens of drugs, including some blood pressure meds and cholesterol drugs. A single glass can cause drug levels to stay high for days. That’s why your pharmacist asks what you eat and drink-not because they’re being nosy, but because they’re trying to keep you alive.

Why Some Side Effects Show Up Days Later
You might think side effects happen right away. But sometimes they sneak in hours-or even days-after you take the drug. That’s because of active metabolites. Take diazepam (Valium). It breaks down into a second drug called desmethyldiazepam, which lasts up to 100 hours. In younger people, it clears out fast. In older adults or those with liver disease? It builds up. That’s why elderly patients on long-term benzodiazepines often fall, get confused, or seem "out of it"-even if they haven’t taken a dose in two days.The same thing happens with codeine. It’s not active itself. Your liver turns it into morphine. If you’re a fast metabolizer? You get strong pain relief. If you’re slow? You get nothing. But if you’re a super-fast metabolizer? You turn codeine into morphine so quickly, you overdose without even knowing it. This isn’t rare. It’s genetic. And it’s why doctors now test for CYP2D6 before prescribing certain drugs.
What Happens When Your Kidneys or Liver Are Weak
Your kidneys are the main exit ramp for most drugs. Normal kidney function clears drugs at a rate of 90-120 mL per minute. But if you have kidney disease, that drops below 15 mL/min. At that point, drugs like vancomycin (an antibiotic) or digoxin (for heart failure) start piling up. One real case from a Reddit pharmacist: a 78-year-old woman with kidney clearance of 25 mL/min was given a standard vancomycin dose. Within days, her creatinine levels shot up from 1.2 to 3.4-signaling kidney damage. She didn’t need more antibiotics. She needed less. But her dose wasn’t adjusted because the system didn’t flag her risk.This is why doctors use formulas like Cockcroft-Gault to estimate kidney function. But here’s the problem: if your weight or age is wrong in the system, the calculation is wrong. A 2022 study found that 15-20% of hospital records had errors in these inputs. That means doses are being miscalculated-on purpose or by accident.
Personalized Dosing Is the Future-And It’s Already Here
We’re moving away from "one-size-fits-all" dosing. In 2021, the FDA approved the first AI-powered dosing tool called DoseMeRx. It uses your age, weight, kidney function, genetics, and even what you ate to calculate your perfect dose. In trials, it cut vancomycin dosing errors by 62%. That’s not a small win. It’s life-saving.Some drugs now require genetic testing before you can even get them. Abacavir, used for HIV, can cause a deadly allergic reaction in people with a specific gene (HLA-B*5701). Screening for this gene prevents 90% of those reactions. Clopidogrel (Plavix), used after heart attacks, doesn’t work well in 30% of people because of a CYP2C19 gene variant. Testing for it cuts the risk of stent clots by 30%.
The NIH just launched a $185 million project to fix a huge blind spot: most pharmacokinetic studies are done on young, white, male volunteers. But 85% of real-world patients are women, older adults, or people of color. We don’t know how drugs behave in these groups. That’s changing. And it’s going to save lives.
What You Can Do Right Now
You don’t need to be a scientist to protect yourself. Here’s what actually works:- Know your meds. Ask your pharmacist: "Is this drug processed by the liver or kidneys?" If it’s one or the other, ask if your liver or kidney function has been checked recently.
- Keep a list. Write down every pill, supplement, and herb you take. Grapefruit, St. John’s wort, and even high-fiber foods can interfere with absorption.
- Ask about timing. Some drugs need to be taken on an empty stomach. Others need food. Get it wrong? You might get no effect-or too much.
- Speak up if something feels off. If you’re tired, dizzy, nauseous, or confused after starting a new drug, don’t assume it’s "just part of aging." It might be a pharmacokinetic issue.
The goal isn’t to scare you. It’s to empower you. Drugs are powerful tools-but they’re not harmless. When you understand how your body handles them, you stop being a passive patient. You become a partner in your care. And that’s the best defense against side effects.
What is pharmacokinetics?
Pharmacokinetics is the study of how your body absorbs, distributes, metabolizes, and excretes drugs. It’s often summarized as "what the body does to the drug," and it determines how much of the drug reaches your target tissues and how long it stays active.
Why do some people have side effects and others don’t?
Differences in genetics, age, liver and kidney function, diet, and other medications all affect how drugs are processed. For example, 3-10% of people have a gene variant that makes them poor metabolizers of codeine, so it doesn’t work for them. Others metabolize it too fast and risk overdose. Even small changes in kidney function can cause dangerous drug buildup.
Can food affect how my medication works?
Yes. Grapefruit juice blocks enzymes that break down over 85 drugs, including statins and blood pressure meds, causing toxic levels. High-fiber foods can delay absorption of some antibiotics. Taking certain drugs with food can either help or hurt-always follow your pharmacist’s instructions.
Why does my doctor keep changing my dose?
Dose changes aren’t arbitrary. They’re based on how your body handles the drug. If your kidney function drops, your dose must go down. If you start a new antibiotic that blocks liver enzymes, your dose might need to be lowered to avoid toxicity. These aren’t mistakes-they’re necessary adjustments.
Is genetic testing for drugs worth it?
For some drugs, yes. Testing for genes like HLA-B*5701 before taking abacavir prevents life-threatening allergies. Testing for CYP2C19 before prescribing clopidogrel cuts the risk of heart stent failure by 30%. These tests are now standard for specific drugs, and they’re covered by most insurance.
How can I tell if a side effect is from a drug or something else?
Track when it started. If symptoms began within days of starting a new medication, it’s likely related. Common red flags: dizziness, confusion, nausea, rash, unusual fatigue, or swelling. Bring your full medication list to your doctor-including supplements. Even natural products can cause serious interactions.

Ernie Simsek
February 14, 2026 AT 11:05Joanne Tan
February 15, 2026 AT 02:55Reggie McIntyre
February 16, 2026 AT 08:45Carla McKinney
February 16, 2026 AT 21:08Jason Pascoe
February 18, 2026 AT 18:19Annie Joyce
February 20, 2026 AT 04:05Rob Turner
February 21, 2026 AT 01:41Craig Staszak
February 22, 2026 AT 12:18alex clo
February 23, 2026 AT 21:09Alyssa Williams
February 23, 2026 AT 22:24