Biosimilar Coding: What It Means for Your Prescriptions and Costs
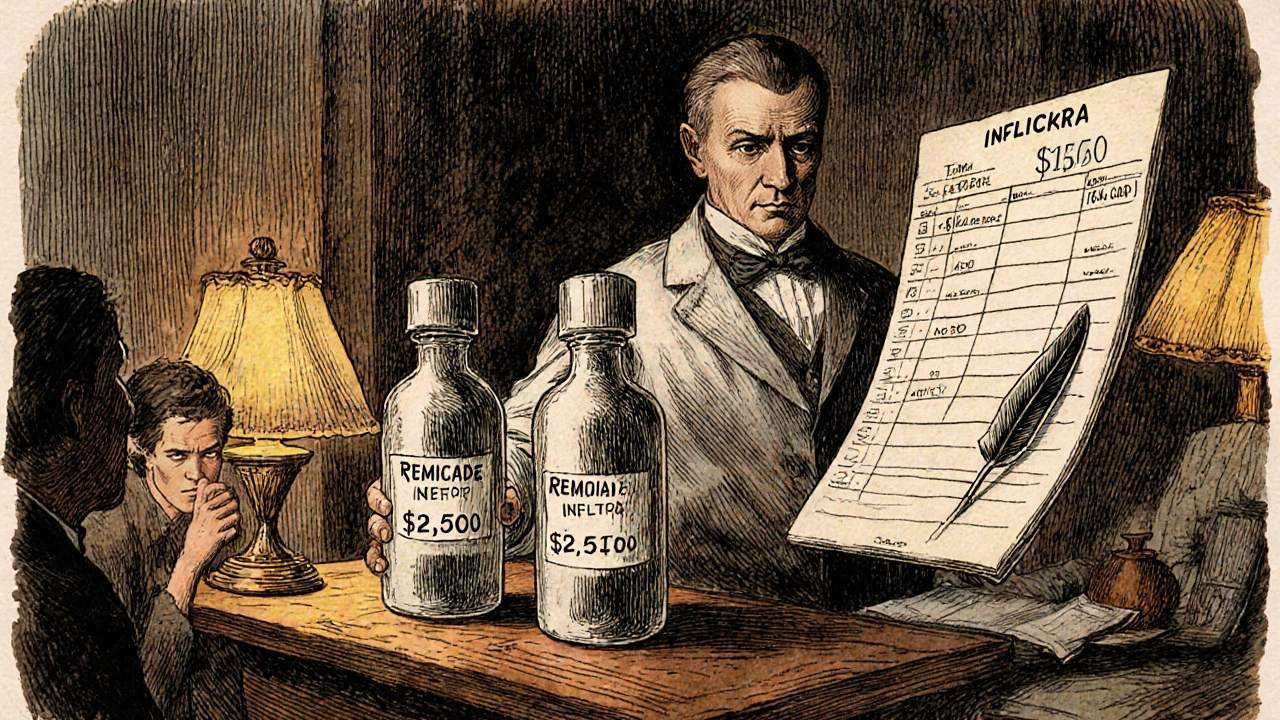
When you hear biosimilar coding, the system that assigns unique identifiers to biologic drugs that mimic brand-name treatments. Also known as biologic product coding, it’s how pharmacies and insurers track which version of a complex drug you’re getting—whether it’s the original or a cheaper copy. Unlike regular generics, biosimilars aren’t exact copies. They’re made from living cells, so even tiny differences in manufacturing can change how they behave in your body. That’s why coding matters: it ensures doctors, pharmacists, and insurers know exactly what’s being prescribed and dispensed.
These codes aren’t just paperwork. They tie directly to generic drug substitution, rules that let pharmacists swap brand-name drugs for lower-cost versions. But with biosimilars, substitution isn’t automatic. Some states require the prescriber to specifically allow it, while others let pharmacists switch unless the doctor says no. This patchwork of rules means your experience in New York might be totally different from your cousin’s in Texas. And because biosimilars often cost 15% to 35% less than the original, getting the right code on your prescription can save you hundreds a year.
Behind the scenes, pharmacy coding, the system that labels drugs with barcodes and identifiers for tracking. Also known as drug identification systems, it’s what stops a pharmacist from accidentally giving you the wrong version. Barcode scanning, which prevents up to 93% of medication errors, relies on these codes to match the right drug to the right patient. If the biosimilar’s code doesn’t match the one on your prescription, the system flags it—and that’s a good thing. It keeps you safe.
But here’s the catch: not all biosimilars are created equal. Some are approved for the same uses as the original, others aren’t. That’s where therapeutic equivalence, a rating that says one drug can be safely swapped for another without losing effectiveness. Also known as drug interchangeability, it’s the key to knowing whether a biosimilar can truly replace the brand. The FDA gives some biosimilars an "A" rating—meaning they’re interchangeable. Others get no rating at all. That’s why your doctor might still prescribe the original, even if a cheaper version exists.
And it’s not just about price. Biosimilar coding affects refill patterns, insurance approvals, and even how your medical records are updated. If your prescription switches from the brand to a biosimilar without you knowing, your doctor might think the treatment isn’t working—when it’s just a different code in the system. That’s why it’s worth asking: "Is this a biosimilar? What’s the code?" It’s not just bureaucracy—it’s your health.
Below, you’ll find real guides that break down how drug substitution works in your state, what labels to check, how pharmacies track these drugs, and why some prescriptions still come with surprises. No fluff. Just what you need to make sure you’re getting the right treatment at the right price.