Biosimilar Reimbursement: How Payors Decide What’s Covered
When you hear biosimilar reimbursement, the process by which insurance plans cover biologic drugs that are highly similar to brand-name versions but cost less. Also known as biologic drug coverage, it’s the quiet engine behind lower prescription prices for millions. Unlike regular generics, biosimilars aren’t exact copies—they’re complex proteins made in living cells, so getting them approved and paid for takes more work. But when insurers do cover them, patients save big. In the U.S., biosimilar reimbursement has cut costs for drugs like Humira and Enbrel by 30% to 50%, and that savings is spreading to other conditions like rheumatoid arthritis, Crohn’s, and even certain cancers.
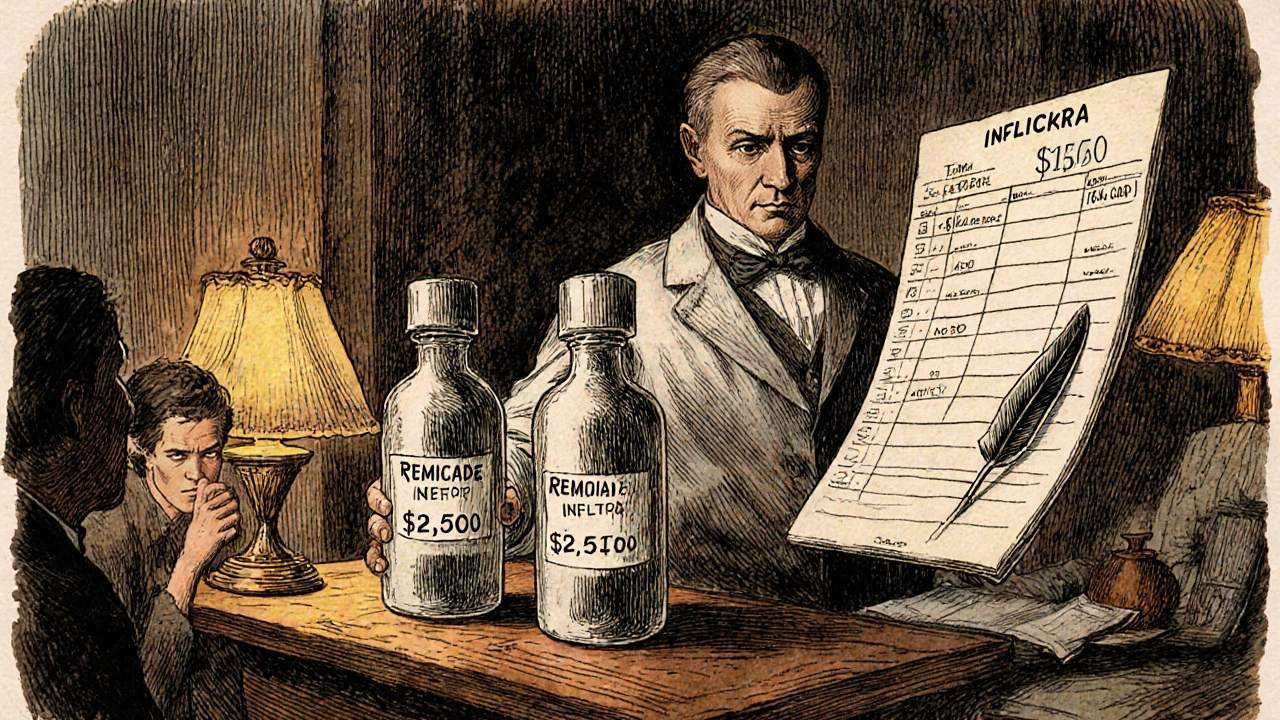
It’s not just about price. insurance coverage, the rules set by health plans and government payors that determine which drugs patients can access at lower cost. Some plans require you to try a biosimilar before approving the brand-name version—this is called step therapy. Others won’t cover a biosimilar unless the doctor checks a box saying it’s medically appropriate. And then there’s the drug pricing, the system of manufacturer discounts, rebates, and negotiated rates that determine what insurers actually pay. Even if a biosimilar is cheaper on the shelf, the manufacturer might offer a rebate to the insurer that makes the brand drug look like the better deal. That’s why you might get denied coverage even if the biosimilar is listed as preferred.
These rules aren’t the same everywhere. State laws, Medicare Part B, and private insurers each have their own policies. Some states require pharmacists to notify you if they switch your drug to a biosimilar. Others don’t. Some plans cover biosimilars at the same tier as the original—meaning your copay doesn’t change. Others push you into a lower tier to encourage use. And while the FDA says biosimilars are as safe and effective as the originals, not every doctor trusts them yet. That’s why so many posts on this site talk about generic drugs, substitution rules, and how pharmacy systems handle these switches.
What you’ll find below are real-world stories and breakdowns of how this plays out: how pharmacists navigate substitution laws, why some patients get stuck paying more even when biosimilars exist, and how the distribution system hides the real cost savings. You’ll see how reimbursement rules affect access to drugs like insulin, rheumatoid arthritis treatments, and even cancer therapies. This isn’t theory—it’s what happens when complex biology meets insurance paperwork. And if you’ve ever been told your prescription changed without your consent, or wondered why your copay jumped even though the drug is "cheaper," these posts will show you why.