Biosimilars Billing: How It Works and What You Need to Know
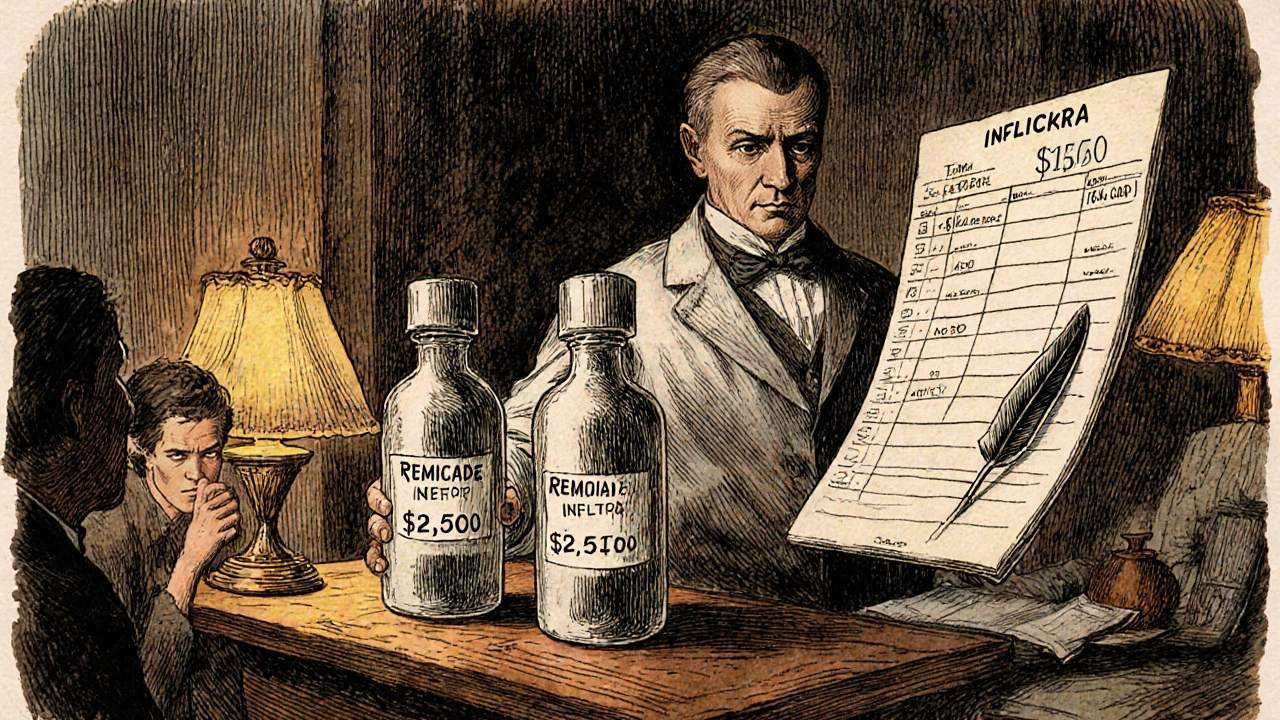
When you hear biosimilars, biologic drugs that are highly similar to an already-approved reference product, often used for autoimmune diseases and cancer. Also known as biologic generics, they offer major cost savings but come with tricky billing rules. Unlike regular generics, biosimilars aren’t exact copies—they’re made from living cells, which means their manufacturing, tracking, and reimbursement are handled differently. That’s why biosimilars billing is one of the most confusing parts of modern pharmacy practice.
Pharmacists and providers have to navigate special HCPCS codes, unique billing identifiers assigned by CMS for biologics and biosimilars to get paid correctly. For example, a biosimilar for rheumatoid arthritis might use a different code than the brand-name version, even if they work the same way. Insurance companies and Medicare use these codes to decide reimbursement rates—and if the wrong one is used, the claim gets denied. That’s not just a paperwork issue; it can delay treatment for patients who rely on these drugs.
Then there’s the three-tier distribution system, the network of manufacturers, wholesalers, and pharmacies that moves drugs from factory to patient. With biosimilars, each step adds layers of pricing complexity. Wholesalers might buy in bulk at deep discounts, but pharmacies still get paid less than for brand-name biologics. That’s why some clinics hesitate to switch—billing systems aren’t always updated, and staff don’t always know how to code them right. And with state drug substitution laws, rules that let pharmacists swap brand drugs for generics or biosimilars without prescriber approval varying across the U.S., what’s allowed in one state might be blocked in another.
Patients often don’t realize their insulin, Humira, or Enbrel might now be a biosimilar—and if they see a lower copay, they assume everything’s fine. But billing errors can mean higher out-of-pocket costs later, or even a denial of coverage. The system is improving, but slowly. New rules in 2025 are pushing for better tracking, clearer labeling, and more transparent pricing. But until then, the people handling the bills—pharmacists, billing clerks, and even patients—are stuck sorting through the mess.
What you’ll find below are real, practical guides from people who’ve dealt with this firsthand: how to read your pharmacy bill, what to do when a biosimilar claim gets rejected, how to spot coding errors, and which states make substitution easier. No theory. No fluff. Just what works when the system doesn’t.