HCPCS Codes for Biosimilars: What You Need to Know
When you hear HCPCS codes, a standardized system used in the U.S. to identify medical supplies, equipment, and drugs for billing. Also known as Healthcare Common Procedure Coding System, it’s the language pharmacies, insurers, and Medicare use to track what’s given to patients and how much they’re paid for it. For biosimilars, biologic drugs that are highly similar to an already-approved reference product, but not exact copies. These are not traditional generics—they’re made from living cells, not chemicals, and require complex manufacturing and testing. That’s why they need their own unique HCPCS codes. Unlike a generic pill like metformin, which shares the same code as its brand-name version, biosimilars get their own distinct codes because they’re treated as separate products by payers and regulators.
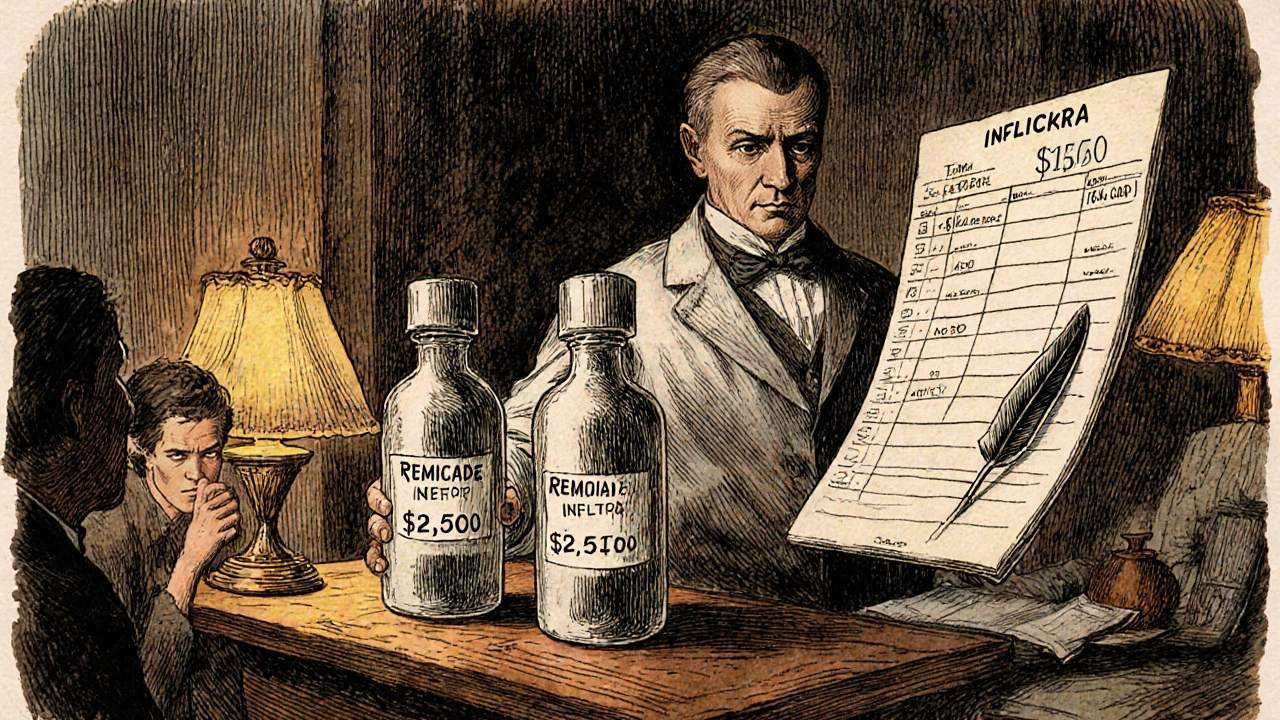
Why does this matter to you? If you’re on a biosimilar for rheumatoid arthritis, Crohn’s, or cancer, your pharmacy and insurer rely on the right HCPCS code to process your claim. Get the code wrong, and your prescription might be denied, delayed, or billed to you at full price. The most common biosimilars—like adalimumab (Humira biosimilars), bevacizumab (Avastin biosimilars), and infliximab (Remicade biosimilars)—each have specific HCPCS Level II codes starting with J- or Q-. These codes link directly to Medicare Part B reimbursement rates and private insurance formularies. Even small coding errors can trigger audits or payment delays that affect both providers and patients.
There’s also a big difference between biosimilars and generic drugs. While generics are chemically identical to brand-name pills, biosimilars are only highly similar to their biologic originals. Because they’re made from living organisms, tiny variations can occur in manufacturing. That’s why the FDA requires extra testing, and why HCPCS codes don’t merge them with the original product. This distinction keeps the system transparent and ensures payers know exactly what they’re covering. You’ll see this reflected in the posts below: some cover how state laws affect substitution, others explain drug pricing, and a few dig into how distribution systems impact access—all tied to the same underlying issue: how complex biologics are coded, paid for, and tracked in real-world care.
What you’ll find here isn’t theory—it’s practical, real-world insight. From how pharmacists verify the right biosimilar code during dispensing, to why some insurers still push back on switching patients, to how Medicare’s payment rules shape what’s available in your pharmacy—these posts cut through the noise. You’ll learn what to ask your provider, how to spot billing errors, and why a single code can make the difference between affordable care and a surprise bill. This isn’t just about paperwork. It’s about making sure you get the right treatment at the right price, without getting lost in the system.