Healthcare Shortages: Why Medications Run Out and What It Means for You
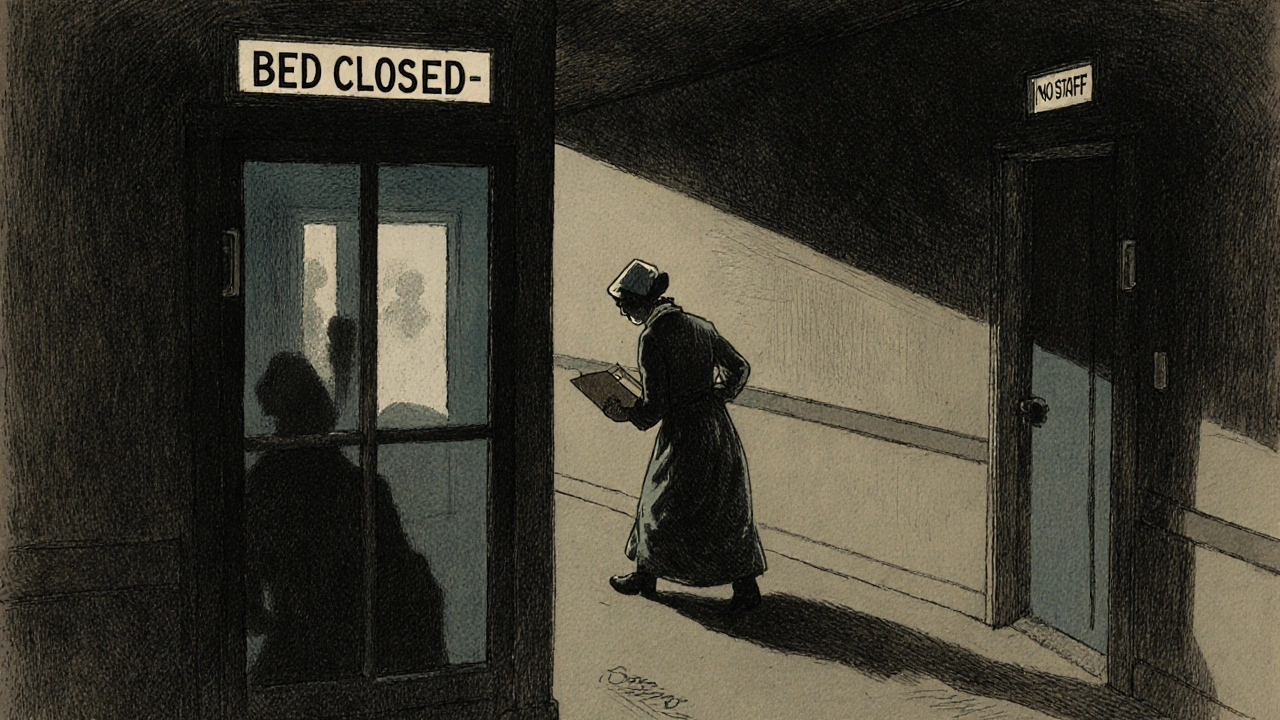
When you need a medication and it’s simply not there, it’s not just frustrating—it’s dangerous. Healthcare shortages, the failure of the supply system to deliver essential medicines to patients. Also known as drug shortages, they happen when manufacturers can’t produce enough, raw materials vanish, or distribution breaks down. This isn’t rare. In the U.S. alone, over 300 drugs faced shortages in 2023, including antibiotics, insulin, and even basic IV fluids. These aren’t niche treatments—they’re the medicines people rely on to survive.
Pharmaceutical supply chain, the network of manufacturers, wholesalers, and pharmacies that moves drugs from labs to your medicine cabinet. It’s fragile. Most generic drugs are made overseas, often in just one or two factories. If one plant shuts down for inspection, or if a key ingredient gets blocked by trade rules, the whole system stumbles. Generic drug pricing, the low-cost model that makes medicines affordable but leaves little room for error. When companies compete on price alone, they cut corners on inventory, storage, and backup plans. A $0.10 savings per pill means nothing if you can’t get the pill at all.
It’s not just about cost. Medication access, whether patients can actually get the drugs they’re prescribed. is affected by hoarding, bulk buying by hospitals, and even panic restocking after news of a shortage. You might see a drug available at one pharmacy but not another—not because it’s out of stock everywhere, but because some buyers get priority. And when a life-saving antibiotic or asthma inhaler disappears, people turn to unsafe alternatives, delay treatment, or worse—go without.
The posts below don’t just talk about shortages—they show you how they connect to real-world problems. You’ll find out why liquid antibiotics expire so fast after mixing, how wholesalers profit from scarcity, why vaccine generics don’t exist like regular ones, and how barcode scanning in pharmacies tries to stop errors when supplies are low. You’ll see how drug interactions become riskier when you’re forced to switch brands, and how expired EpiPens or patches are handled when replacements aren’t coming. This isn’t theory. It’s what’s happening in pharmacies right now, and you deserve to know why.