Medicare Part B Biosimilars: What You Need to Know About Cost-Saving Alternatives
When you’re on Medicare Part B biosimilars, FDA-approved versions of complex biologic drugs that are highly similar to brand-name versions but cost significantly less. These aren’t generic pills—they’re advanced, lab-made treatments for conditions like rheumatoid arthritis, cancer, and diabetes. Unlike traditional generics, which copy simple chemical formulas, biosimilars replicate large, intricate proteins made from living cells. That’s why they’re called biosimilars, biological products that are highly similar to an approved reference product with no clinically meaningful differences in safety or effectiveness. They’re not exact copies, but they work the same way—and they’re approved by the same strict standards as the originals.
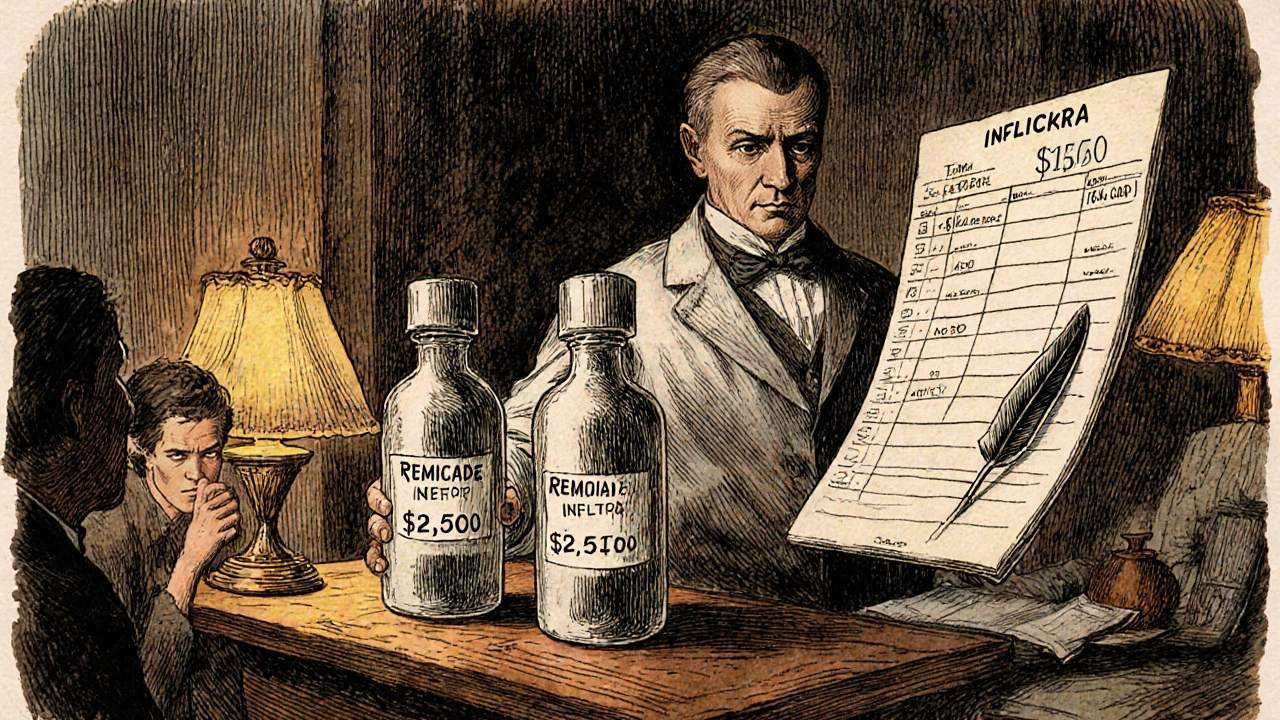
Medicare Part B covers many of these drugs when given in a doctor’s office or clinic, which is different from Part D that handles self-administered pills. That means if you’re getting a biosimilar infusion for Crohn’s disease or a biosimilar injection for multiple sclerosis, Medicare Part B pays most of the cost. You still pay your 20% coinsurance, but the total bill drops dramatically compared to the brand-name version. For example, a biosimilar for a common arthritis drug might cost $5,000 instead of $15,000 per year. That’s not a small difference—it’s life-changing for people on fixed incomes. And because biosimilars are entering the market faster now, more options are becoming available every year. They’re not just cheaper—they’re expanding access to treatments that were once out of reach.
There’s a common myth that biosimilars are "lesser" drugs. They’re not. The FDA requires them to go through years of testing—comparing them directly to the original biologic in clinical trials, measuring immune response, checking for side effects, and proving they work just as well. In fact, millions of people in the U.S. and Europe have used biosimilars safely for over a decade. What’s changing now is that Medicare is pushing providers to switch to biosimilars where possible, because the savings help the whole system. Pharmacists can substitute them automatically in many cases, just like with regular generics. And if your doctor prescribes a brand-name biologic, you can ask: "Is there a biosimilar option?" It’s your right to know.
You’ll find posts here that dig into how biosimilars fit into real-world care—like how they interact with other meds, what insurance hurdles you might face, and why some doctors still hesitate to prescribe them. You’ll also see how these drugs compare to traditional generics, how storage and handling differ, and what to watch for if you switch from a brand-name drug. This isn’t theoretical. These are the questions people are asking at pharmacies, clinics, and kitchen tables across the country. The goal? To help you get the right treatment without paying more than you have to.