Nurse Shortage: Why It's Hitting Harder Than Ever and What It Means for Your Care
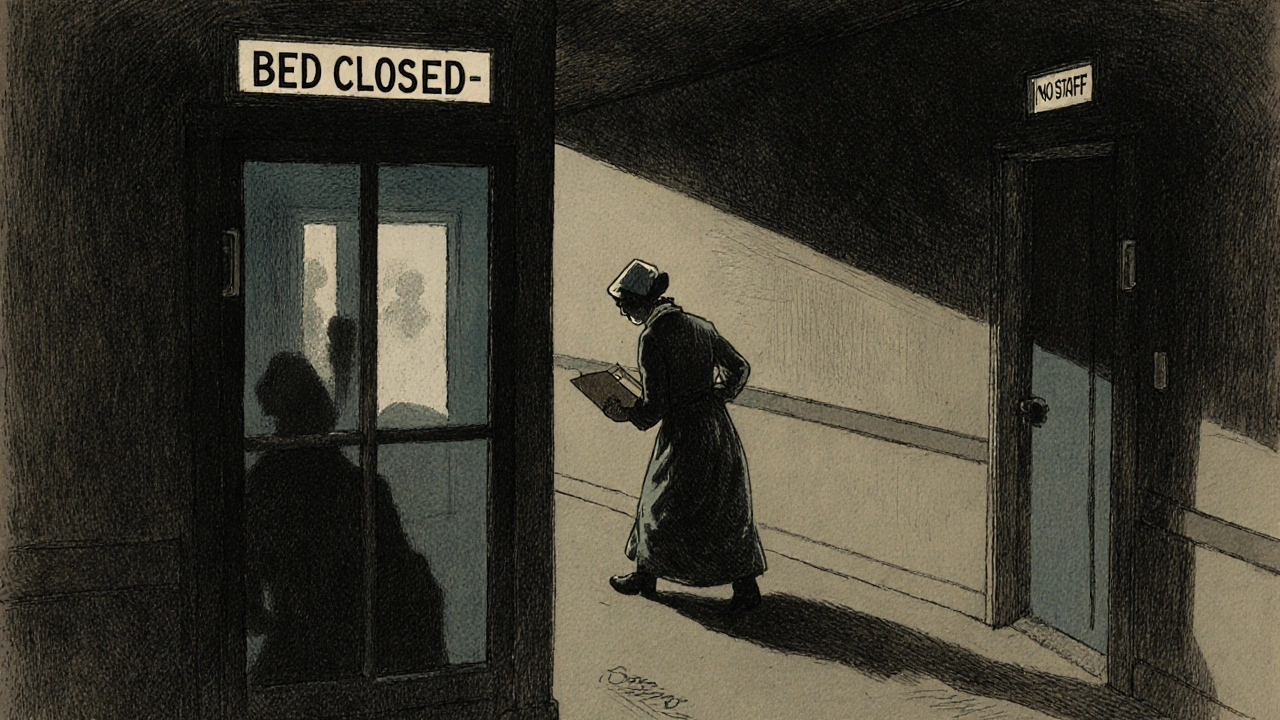
When you walk into a hospital or clinic, you expect trained professionals to be there—someone who knows your meds, notices your pain, and asks the right questions. But that’s becoming harder to count on. The nurse shortage, a critical gap between the number of nurses needed and the number available to provide care. Also known as healthcare staffing crisis, it’s not just a backroom issue—it’s what delays your treatment, cuts your visit short, and leaves families scrambling for answers. This isn’t a future problem. It’s happening now, in every state, in every type of facility—from big city hospitals to rural clinics that haven’t had a full-time nurse on staff for months.
The nursing workforce, the group of registered nurses, licensed practical nurses, and nurse assistants who deliver day-to-day care is aging fast. Nearly half of all nurses in the U.S. are over 50, and many are retiring. At the same time, schools can’t train enough new nurses to replace them. Nursing programs turn away thousands each year because they lack clinical instructors, simulation labs, or even enough hospital placements. And when new nurses do graduate, they’re leaving fast—burnout, impossible workloads, and emotional exhaustion push one in three out of the field within five years. This isn’t just about numbers. It’s about patient safety, the direct link between nurse staffing levels and how often patients get hurt, infected, or miss critical care. Studies show that when nurses have too many patients, mistakes rise—medication errors, missed vital signs, delayed responses to deteriorating conditions. One hospital in Ohio found that when nurse-to-patient ratios jumped from 1:4 to 1:7, falls and infections went up by 32%.
The ripple effects are everywhere. Emergency rooms sit backed up because there aren’t enough nurses to move patients to inpatient units. Home care agencies can’t send nurses to elderly patients who need daily check-ins. Long-term care facilities rely on temporary staff who don’t know your history. Even your primary care doctor might be working with a nurse who’s covering three clinics in one day. The system is stretched thin, and it’s you and your family who feel it first.
What you’ll find in the posts below isn’t just theory—it’s real, practical insight from the front lines. You’ll see how expired medication disposal connects to staffing gaps, why generic drug pricing affects hospital budgets, and how barcode scanning in pharmacies was meant to help—but only if there’s a nurse there to use it. These stories aren’t isolated. They’re all tied to the same broken system. This isn’t about blaming anyone. It’s about understanding what’s really happening so you can ask better questions, advocate for yourself, and know what to expect when you need care the most.