Vaccine Generics: What They Are, How They Work, and Why They Matter
When you hear vaccine generics, copies of brand-name vaccines that meet the same safety and effectiveness standards but cost far less. Also known as biosimilars in some cases, they are the backbone of affordable immunization programs worldwide. These aren’t knockoffs—they’re scientifically identical versions of vaccines like hepatitis B, HPV, or flu shots, made after the original patent expires. The difference isn’t in how they work, but in who makes them and how much they cost.
Behind every vaccine manufacturing, the complex process of producing biological vaccines under strict regulatory controls is a network of labs, quality checks, and cold-chain logistics. Companies in India, China, and Eastern Europe now produce most of the world’s generic vaccines, supplying low-income countries and cutting prices by up to 90%. This isn’t magic—it’s scale, efficiency, and regulatory alignment with WHO and FDA standards. But it’s not easy. Making a safe, stable vaccine requires precision. One wrong temperature, one contaminated batch, and the whole lot gets scrapped. That’s why only a few manufacturers can do it reliably.
Then there’s the vaccine pricing, the cost structure that determines who gets access and who doesn’t. Brand-name vaccines often carry markups that cover R&D, marketing, and shareholder returns. Generic versions strip that away. They don’t need to advertise. They don’t need fancy packaging. They just need to be safe, effective, and cheap. That’s why UNICEF and Gavi can buy millions of doses for under $1 each—enough to vaccinate entire nations. But pricing isn’t always straightforward. Shortages, raw material costs, and export bans can spike prices overnight. And while generics are cheaper, they’re not always available everywhere—especially for newer vaccines like shingles or RSV.
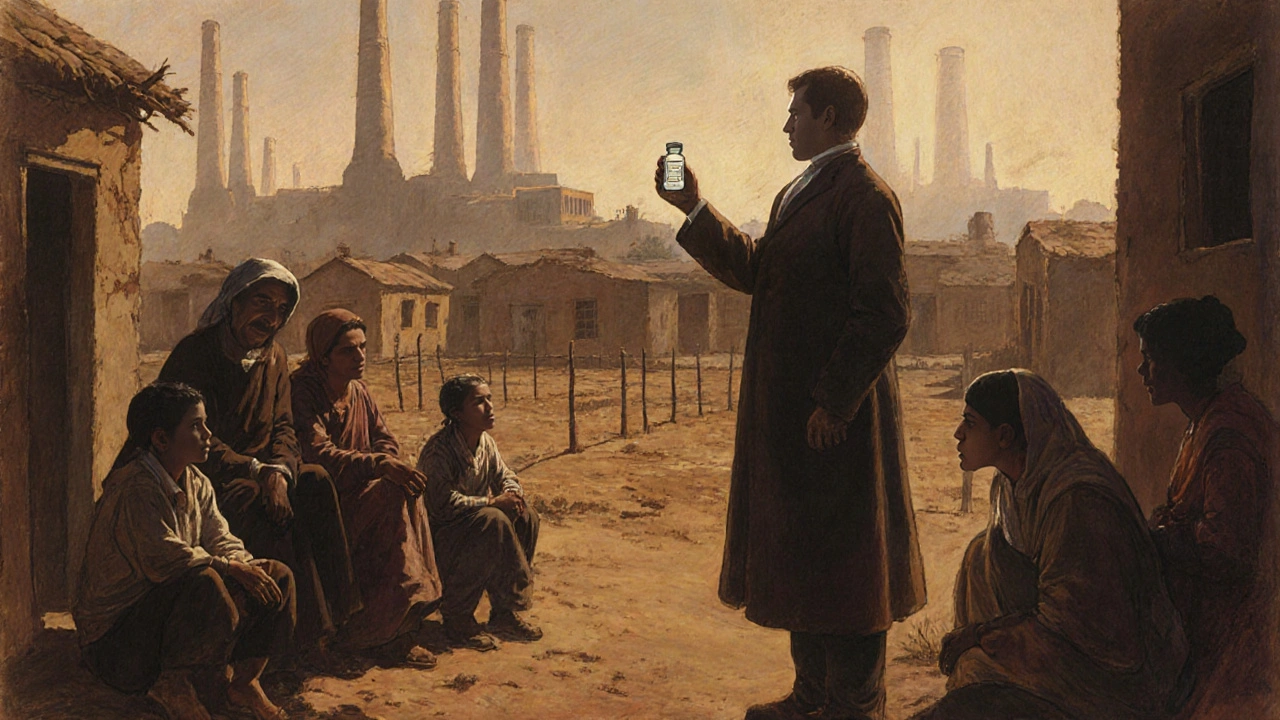
What you won’t find in the fine print is that vaccine generics aren’t just about saving money. They’re about saving lives. In places where a single dose of a brand-name vaccine costs more than a week’s wages, generics make immunization possible. They let schools vaccinate kids. Clinics cover entire villages. Governments run national programs instead of picking and choosing who gets protected. They’re the reason polio is nearly gone and measles outbreaks are easier to contain.
And they’re not going away. As more patents expire and new manufacturers enter the market, the range of available generic vaccines keeps growing. You’ll see them for HPV, pneumococcal disease, even combination shots that used to cost hundreds. The real question isn’t whether they work—it’s whether your healthcare system will make them easy to get.
Below, you’ll find real-world breakdowns of how these vaccines are made, priced, distributed, and why some countries still struggle to access them—even when the science says they should be available to everyone.