When you're on a blood thinner like warfarin, even a small change in your routine can throw your blood off balance. One of the most common but often misunderstood factors? Alcohol. It’s not just about getting drunk. Even a few drinks can cause your INR to spike-or drop-leading to serious bleeding or clotting risks. If you’re taking warfarin, understanding how alcohol affects your blood is not optional. It’s essential.
What Is INR, and Why Does It Matter?
INR stands for International Normalized Ratio. It’s a number doctors use to measure how long it takes your blood to clot. If you’re not on blood thinners, your INR is usually between 0.8 and 1.1. But if you’re taking warfarin, your target range is between 2.0 and 3.5, depending on your condition. For atrial fibrillation, it’s often 2.0-3.0. For a mechanical heart valve, it might be 2.5-3.5. Go above 3.5, and your risk of bleeding jumps. Go below 2.0, and you’re at risk of a clot.
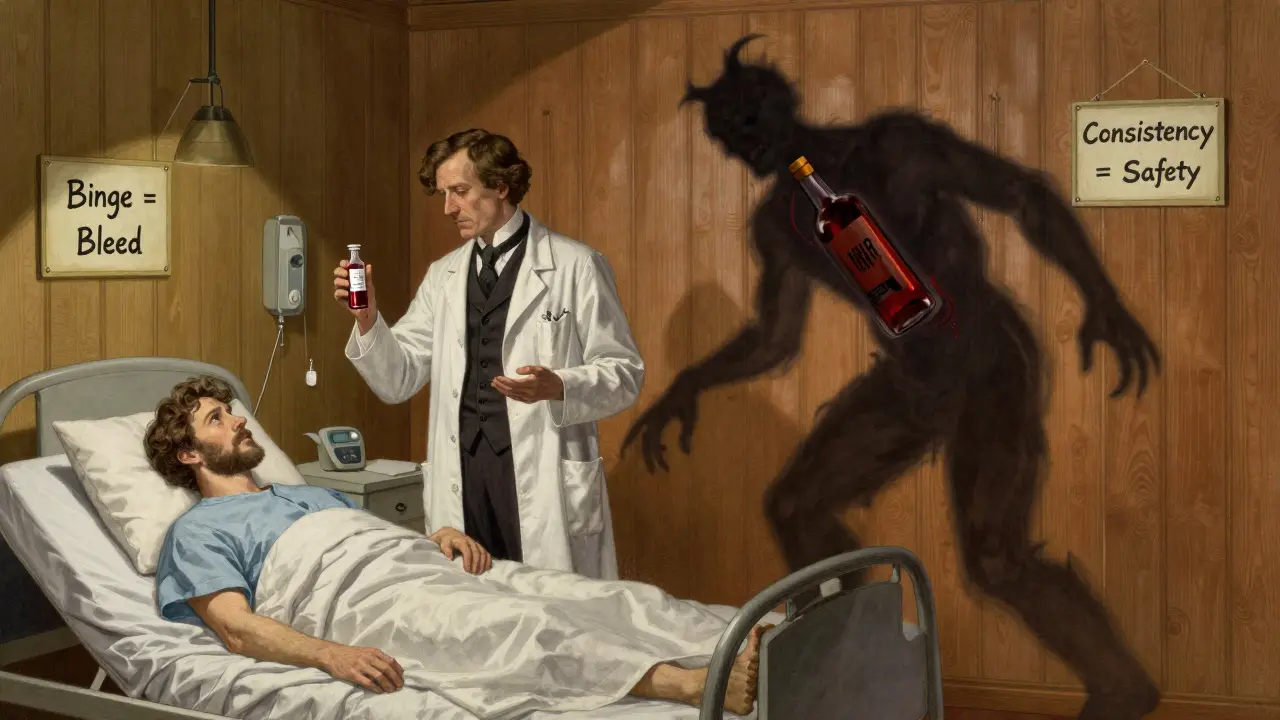
Each 0.5-point increase above your target range raises your bleeding risk by 30-50%. That’s not a small shift. An INR over 9 is life-threatening. Studies show that among hospitalized patients with INR above 9, 35% had serious bleeding, and 17% died. Alcohol is one of the top three reasons INR climbs that high-alongside older age and kidney problems.
How Alcohol Interacts With Warfarin
Warfarin doesn’t work alone. It’s broken down in your liver by enzymes, mainly CYP2C9. Alcohol messes with these enzymes. When you drink, your liver prioritizes clearing alcohol first. That slows down how fast warfarin gets processed. Result? Warfarin builds up in your blood. Your INR rises. Your blood thins too much.
But it’s not that simple. Sometimes, heavy drinking over days or weeks can actually make your liver work harder to break down warfarin. That lowers your INR. Now you’re at risk of clots. One day, alcohol makes your blood thinner. The next, it makes it thicker. That’s why doctors say alcohol causes unpredictable INR changes.
A 2015 NIH study found that people with certain gene variants (CYP2C9*2/*3 and VKORC1 1173G>A) are especially sensitive. Their bodies process warfarin differently. For them, even one drink can trigger a dangerous INR spike. These genetic differences explain why two people can drink the same amount and have totally different outcomes.
Real Stories: When a Drink Turned Dangerous
A 62-year-old man in Sydney was doing fine on warfarin. His INR stayed steady at 2.8. Then he had six pints of beer over a weekend. Within 48 hours, his INR jumped to 5.2. He ended up in the hospital with internal bleeding. His doctor said it wasn’t the beer alone-it was the pattern. Binge drinking, even once, can be deadly.
On Reddit’s r/Warfarin forum, users share similar stories. One person said their INR went from 2.4 to 3.8 after four glasses of wine. Another described nosebleeds that wouldn’t stop after a single cocktail. These aren’t rare cases. In fact, about 30-40% of people on warfarin drink alcohol regularly. That’s millions of people navigating this tightrope.
How Much Alcohol Is Safe?
There’s no magic number that works for everyone. But experts agree on this: consistency beats quantity.
The British Heart Foundation says it’s okay to drink alcohol on warfarin-as long as you stick to the UK guidelines: no more than 14 units per week, spread over three or more days. One unit equals half a pint of beer, a small glass of wine, or a single shot of spirits.
Medical News Today defines heavy drinking as more than 14 drinks a week for men, or 7 for women. That’s not a target-it’s a red line. Exceeding it raises your bleeding risk significantly.
Here’s what works in real life:
- Stick to 1-2 drinks on occasion, not every day.
- Avoid binge drinking-no more than 3 drinks in one sitting.
- Don’t skip your INR checks if you’ve had alcohol.
- Keep your drinking pattern the same week to week. If you drink on weekends, do it every weekend. If you don’t, don’t start.
Why consistency? Because your liver adapts. If you drink the same amount regularly, your body adjusts. If you go from zero to six drinks in one night, your INR swings wildly. That’s when trouble starts.
What About Newer Blood Thinners?
Many people now take DOACs-direct oral anticoagulants-like apixaban, rivaroxaban, or dabigatran. These drugs don’t need regular INR checks. And they interact less with alcohol than warfarin.
But that doesn’t mean they’re safe with heavy drinking. Alcohol still increases bleeding risk on its own. It can irritate your stomach lining, cause falls, or make you forget your pill. One study found that even on DOACs, heavy drinkers had a higher chance of bleeding than non-drinkers.
And here’s the catch: if you bleed badly on a DOAC, there’s no quick fix. Warfarin can be reversed with vitamin K or plasma. DOACs? Only a few have reversal agents, and they’re expensive and hard to get quickly.
If you’re on a DOAC, moderation still matters. The safest choice? Keep alcohol light and steady.
Warning Signs: When to Seek Help
Don’t wait for a crisis. Know the signs of internal bleeding:
- Red or brown urine
- Tar-like or bright red stools
- Bleeding gums or nosebleeds that won’t stop
- Unusual bruising without injury
- Heavier-than-normal menstrual bleeding
- Brown or bright red vomit
- Sudden headaches, dizziness, or weakness
If you notice any of these after drinking-even if you think it’s "just a little"-call your doctor or go to the ER. INR levels can spike fast. Waiting could cost you your life.
What Your Doctor Wants You to Do
Your doctor isn’t trying to take away your social life. They want you to live safely. Here’s what they expect:
- Tell them if you drink alcohol-no shame, no hiding.
- Keep your alcohol intake consistent. No sudden changes.
- Get your INR checked more often if you’ve had alcohol recently.
- Use telehealth services if available. Some programs now include alcohol counseling and real-time INR tracking. Patients using these services saw a 25% drop in complications.
- Don’t rely on online advice. Your situation is unique.
Warfarin is still prescribed to over 2.5 million Americans every year. Even with newer drugs available, it’s cheap, effective, and well-understood. But it demands respect. Alcohol isn’t the enemy. Unpredictable, inconsistent drinking is.
Bottom Line: Drink Smart, Not Hard
You don’t have to give up alcohol to stay safe on warfarin. But you do have to be smart. One drink now and then? Fine. Six drinks on a Friday night? Dangerous. Binge drinking? Life-threatening.
The goal isn’t perfection. It’s control. Control your intake. Control your timing. Control your monitoring. If you do that, you can enjoy a drink without risking a bleed.
And if you’re unsure? Ask your doctor. Bring your alcohol habits to your next appointment. Write it down. Track it. Your INR will thank you.


kabir das
January 30, 2026 AT 10:33Wait-so if I have one glass of wine every Friday, and then suddenly have two on a Saturday because my cousin visited… my INR could go nuts?? I’ve been doing that for years. I’m 68, on warfarin since my stroke in ’19… and I just assumed consistency meant “not getting drunk.” But now I’m sweating. My last INR was 2.9. Should I call my doctor tomorrow? Or just quit wine??
DHARMAN CHELLANI
February 1, 2026 AT 06:53lol so much fearmongering. you think your liver is some delicate flower? i drink 3 beers a night, 7 days a week. INR 2.6. always. my doc says ‘if it aint broke dont fix it.’ also, warfarin is for peasants. DOACs are for people who actually know what they’re doing. ps: you spelled ‘alcohol’ wrong. again.
Laura Arnal
February 2, 2026 AT 16:36Thank you for this!! 🙌 I’m on apixaban and still drink 1 glass of wine 3x/week. I used to panic every time I had a drink-now I just track it in my app and keep it steady. You’re right: consistency > quantity. And yes, even DOACs aren’t magic. Stay smart, stay safe. You’ve got this! 💪🍷
Eli In
February 3, 2026 AT 19:55As someone who moved from India to the US and had to relearn how to drink (and why I shouldn’t), this hit home. 🌍 In Delhi, we had a drink with dinner every night-no big deal. Here, I learned the hard way that ‘no big deal’ doesn’t translate to warfarin. I now have a tiny wine glass on my counter as a reminder. Small, slow, steady. 🥂❤️
Ryan Pagan
February 5, 2026 AT 08:17Let’s be real-alcohol doesn’t care about your INR. Your liver does. And if your liver is tired, stressed, or overloaded with pizza and Netflix, that one glass? It’s not a glass-it’s a sledgehammer. I’ve seen patients go from ‘fine’ to ICU in 48 hours after a weekend bender. You think you’re ‘just having fun’? Your clotting factors are screaming. Don’t be the guy who says ‘I didn’t know.’ You knew. You just didn’t care enough to change.
Paul Adler
February 5, 2026 AT 10:29This is a well-researched and thoughtful summary. The emphasis on behavioral consistency rather than absolute abstinence is clinically sound and humane. Many patients abandon monitoring or medication because they feel demonized-not because they’re reckless. Framing this as a matter of rhythm, not restriction, increases adherence. Kudos to the author for recognizing that.
Robin Keith
February 5, 2026 AT 18:34And yet… here we are, in the postmodern paradox of medicalized existence: we are told to control our bodies with algorithmic precision, yet our very biology-our enzymes, our genes, our liver’s quiet rebellion against societal norms-refuses to be quantified. Alcohol, in its ancient, Dionysian wisdom, reminds us that we are not machines. But then again… if your INR spikes to 9.2, and you’re bleeding into your peritoneum… well… maybe the machine is right. Maybe the algorithm knows better than your weekend bender. Maybe your soul isn’t worth the clot. Or the bleed. Or the funeral. I weep for the human condition.
Sheryl Dhlamini
February 7, 2026 AT 00:00I used to think ‘one drink’ was harmless. Then I had a nosebleed that lasted 47 minutes after a single margarita. I didn’t even realize it was related until my ER doc asked, ‘Do you drink?’ I said ‘sometimes.’ He said, ‘That’s the problem.’ I haven’t had a drink since. Not because I’m perfect… but because I don’t want to die over a cocktail.
Doug Gray
February 7, 2026 AT 11:48Interesting. The pharmacokinetic modulation of CYP2C9 by ethanol is well-documented, yet the clinical translation remains heterogeneous across populations. The article’s reliance on self-reported data and anecdotal Reddit narratives introduces significant selection bias. Also, the recommendation to ‘track it’ is vague-what’s the operational definition of ‘track’? A journal? An app? A prayer? The lack of standardized behavioral metrics undermines the entire intervention framework. 🤔
Kristie Horst
February 8, 2026 AT 15:11How delightful. Another article that tells people to ‘be responsible’ while ignoring that responsibility is a luxury. Not everyone has access to weekly INR checks. Not everyone can afford DOACs. Not everyone has a doctor who listens. So yes-‘drink smart’… if you’re lucky enough to have the resources to do so. Otherwise? You’re just a statistic with a wine glass. 😌
LOUIS YOUANES
February 9, 2026 AT 05:41Everyone’s acting like alcohol is the devil. Newsflash: it’s not. It’s a molecule. You’re the one who decides how much you take. If your INR swings, it’s not because of the drink-it’s because you’re inconsistent. And inconsistent people shouldn’t be on warfarin. Period. Get a DOAC. Or quit drinking. Or stop being dramatic.
Andy Steenberge
February 9, 2026 AT 14:23One thing I’ve learned from working with hundreds of patients on anticoagulants: the ones who thrive aren’t the ones who never drink. They’re the ones who tell their doctor the truth. They write it down. They bring their wine bottles to appointments. They say, ‘I had three last weekend.’ And then they get help-not judgment. That’s the real secret. Not abstinence. Honesty. So if you’re reading this and you’ve been hiding your drinks… it’s not too late. Talk to your doctor. They’ve heard it all. And they’re not here to shame you. They’re here to keep you alive.