For many people, anxiety isn’t just feeling nervous before a presentation or worrying about a bill. When it becomes constant, overwhelming, and starts controlling your life, it’s not just stress-it’s an anxiety disorder. These aren’t signs of weakness or overthinking. They’re real, measurable medical conditions backed by decades of research. And the good news? We know exactly how to treat them.
What Are Anxiety Disorders?
Anxiety disorders are more than just feeling anxious. They’re persistent, excessive fear or worry that doesn’t go away-even when there’s no real threat. The Anxiety Disorders are a group of mental health conditions defined by the DSM-5 as persistent, excessive fear or worry in situations that are not threatening. Unlike normal anxiety, which fades after the stressor passes, these disorders last for months, interfere with work, relationships, and even basic tasks like leaving the house.They’re also incredibly common. Nearly 1 in 5 U.S. adults experiences an anxiety disorder each year. Women are nearly twice as likely to be diagnosed as men. And while many assume these conditions start in adulthood, half of all cases begin by age 11. The key isn’t whether you feel anxious-it’s whether that anxiety is out of proportion, lasts too long, and stops you from living your life.
The Seven Main Types of Anxiety Disorders
Not all anxiety looks the same. There are seven distinct types, each with its own pattern of symptoms and triggers.- Generalized Anxiety Disorder (GAD) is the most common. People with GAD worry constantly-about work, health, family, even things they can’t control. This isn’t just being a perfectionist. It’s racing thoughts, sleepless nights, and physical tension that lasts six months or longer. About 3.1% of U.S. adults have GAD.
- Panic Disorder involves sudden, intense panic attacks. These aren’t just bad days. They’re episodes where your heart races to 140 beats per minute, you feel like you’re having a heart attack, you can’t breathe, and you’re terrified you’re losing control. These attacks happen unexpectedly, and then you spend weeks fearing the next one.
- Social Anxiety Disorder isn’t shyness. It’s an overwhelming fear of being judged, embarrassed, or humiliated in everyday situations-talking to a cashier, speaking up in a meeting, even eating in public. About 7.1% of adults live with this.
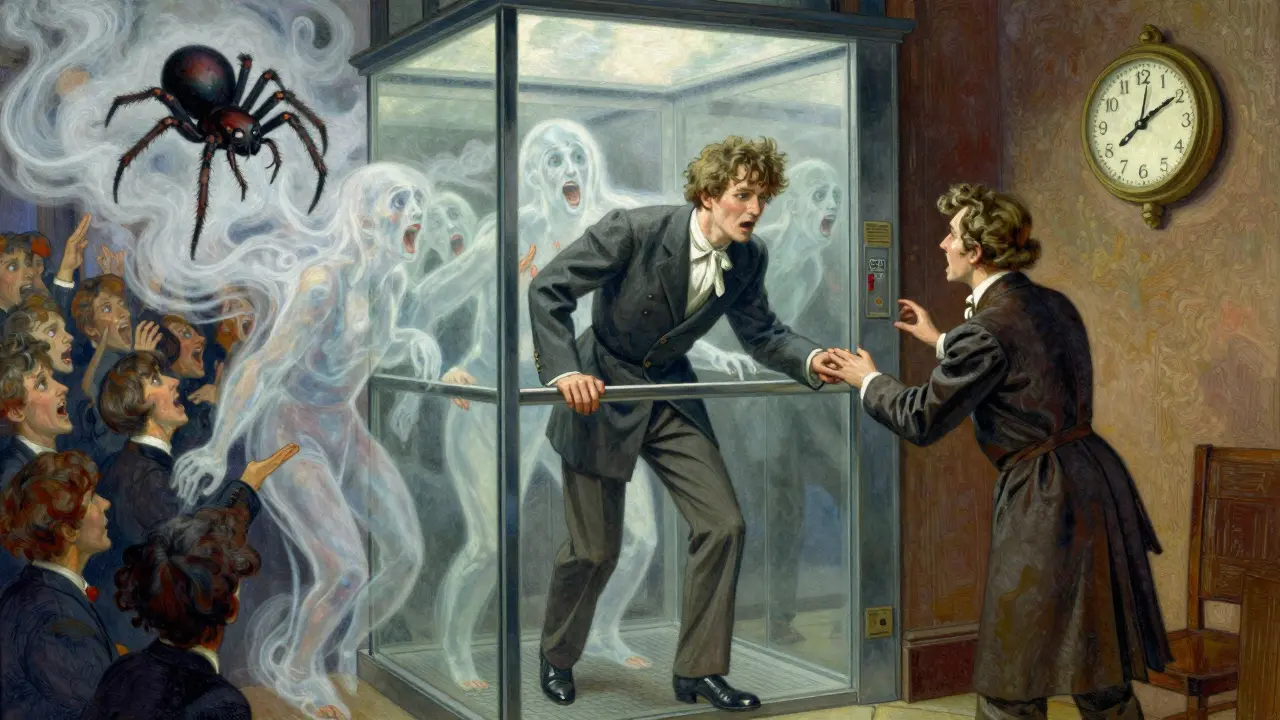
- Specific Phobias are intense fears of specific things: heights, spiders, flying, needles. The fear is so strong that people go out of their way to avoid these triggers, even if they know the danger is minimal. This affects nearly 9% of adults each year.
- Separation Anxiety Disorder used to be seen as a childhood issue. Now we know adults can have it too-fearing being separated from loved ones to the point of panic, even if they’re just going to the store.
- Obsessive-Compulsive Disorder (OCD) is now classified separately, but it still belongs in the anxiety family. It’s not just being tidy. It’s intrusive, unwanted thoughts (obsessions) that cause extreme anxiety, followed by repetitive behaviors (compulsions) to relieve it-like checking locks 20 times or washing hands until they bleed.
- Selective Mutism affects mostly children. They speak normally at home but stay completely silent in school or social settings. It’s not defiance-it’s extreme anxiety locking their voice.
Common Symptoms Across All Types
While each disorder has unique features, they all share physical, cognitive, and emotional symptoms.Physical symptoms include: heart palpitations (often 110-140 bpm during panic), trembling, sweating (reported by 92% of panic disorder patients), shortness of breath (83%), dizziness (76%), nausea (68%), and muscle tension.
Cognitive symptoms are just as real: racing thoughts (82%), difficulty concentrating (89% in GAD), catastrophic thinking (“If I make a mistake, I’ll lose everything”), and rumination-replaying the same worry over and over. One person described it as “a mental hamster wheel that won’t stop.”
Emotional symptoms include feeling like something terrible is about to happen (95% during panic attacks), fear of losing control, and a constant sense of dread. Many say it’s like living with a smoke alarm that won’t stop screaming-even when there’s no fire.
What Works: Evidence-Based Treatments
The most important thing to know: anxiety disorders are treatable. And we know which treatments actually work.Cognitive Behavioral Therapy (CBT) is the gold standard. It’s not just talking. It’s structured, skill-based training. You learn to identify distorted thoughts, face fears gradually (exposure therapy), and use breathing techniques to calm your body. Studies show 50-60% of people see major symptom reduction after 12-20 weekly sessions. For specific phobias and social anxiety, exposure therapy works 60-80% of the time when done correctly.
Medication helps too. SSRIs are selective serotonin reuptake inhibitors like sertraline and fluoxetine, first-line medications for anxiety disorders with 40-60% response rates after 8-12 weeks. They don’t make you feel “happy.” They take the edge off the constant fear so you can actually use therapy tools. Side effects like nausea or emotional numbness can happen-but they often fade after a few weeks. If SSRIs don’t work, SNRIs like venlafaxine are the next step.
Benzodiazepines (like Xanax) work fast-but they’re not for long-term use. They can be addictive, cause memory problems, and make withdrawal worse than the original anxiety. Most guidelines now limit them to short-term crisis use only.
What Doesn’t Work (And Why People Quit)
Many people try treatment and give up. Why? Because it’s hard.Exposure therapy makes you feel worse before it gets better. You might face your fear of elevators-and panic harder than ever. That’s normal. But without knowing why, people think it’s not working and quit.
Medication side effects can be brutal. One Reddit user said, “SSRIs helped my shaking but made me feel like a zombie.” Switching medications or adding buspirone (a non-addictive anti-anxiety drug) often helps.
Access is a huge barrier. In the U.S., wait times for specialized therapists are 6-8 weeks. Insurance often limits therapy to 6-10 sessions. Many people can’t afford the out-of-pocket cost.
And yet-those who stick with it see results. A VA survey found only 37% of people reached remission after six months. But among those who completed full CBT courses, 80% reported major improvement.

New Frontiers in Treatment
The field is moving fast. In 2023, the FDA approved zuranolone (Zurzuvae), the first oral neuroactive steroid approved specifically for postpartum anxiety, with a 54% remission rate in clinical trials. It works differently than SSRIs-targeting brain chemistry directly-and offers relief in days, not weeks.Research is also exploring ketamine-assisted therapy, which showed 65% rapid response in treatment-resistant anxiety in 2022 trials. And AI tools are now predicting panic attacks 24 hours in advance with 87% accuracy-helping people prepare before symptoms hit.
Acceptance and Commitment Therapy (ACT) is now a first-line option alongside CBT. Instead of fighting thoughts, ACT teaches you to notice them without getting swept away-like watching clouds pass without trying to control the sky.
What You Can Do Right Now
You don’t have to wait for a therapist to start feeling better.- Practice diaphragmatic breathing: inhale for 4 seconds, hold for 2, exhale for 6. Do this 5-6 times a minute. It physically calms your nervous system.
- Use a free app like nOCD or Wysa. They offer guided CBT exercises and have been shown to reduce symptoms by 35-45% in 8 weeks.
- Write down your worries. Then ask: “Is this likely? What’s the worst that could happen? And if it did, could I handle it?” Most fears collapse under this kind of scrutiny.
- Find a support group. The Anxiety and Depression Association of America runs 300+ weekly groups. You’re not alone.
Recovery isn’t linear. Some days will feel like progress. Others will feel like backsliding. That’s normal. What matters is that you keep showing up-for therapy, for breathing, for small exposures. You’re not broken. You’re dealing with a medical condition that responds to proven tools. And those tools are more effective than ever.
Can anxiety disorders go away on their own?
Rarely. While some people experience less anxiety as they age, most disorders persist or worsen without treatment. Left untreated, anxiety increases the risk of depression, substance use, and chronic health problems. Early intervention leads to much better long-term outcomes.
Is therapy better than medication for anxiety?
It depends. CBT has longer-lasting effects-people often stay better even after stopping therapy. Medication works faster and helps with severe symptoms. The best results come from combining both. One large study found 58% of people improved with therapy + medication, compared to 42% with medication alone and 38% with therapy alone.
How long does CBT take to work?
Most people start noticing changes in 4-6 weeks. By session 12, 60-80% of patients report significant improvement. It’s not a quick fix-it’s skill-building. Think of it like learning to swim: you won’t float on day one, but with practice, you get stronger.
Can I treat anxiety without medication?
Yes, many people do. CBT, ACT, breathing techniques, regular exercise, and sleep hygiene can be enough for mild to moderate cases. But if symptoms are severe-panic attacks, inability to leave home, extreme avoidance-medication can be a necessary bridge to make therapy possible.
Why do some people say medication made them feel numb?
SSRIs reduce the intensity of all emotions-not just anxiety. Some people describe it as emotional flattening. This often improves over time. If it doesn’t, switching to a different SSRI or trying buspirone (which doesn’t dull emotions) can help. Never stop medication abruptly-talk to your doctor.
Are digital apps for anxiety actually effective?
Yes-especially FDA-cleared ones like nOCD and Wysa. Studies show they reduce symptoms by 35-45% in 8 weeks with daily use. They’re not replacements for therapy, but they’re powerful tools for building skills between sessions, especially when access to a therapist is limited.
Next Steps: Where to Go From Here
If you recognize these symptoms in yourself or someone you care about, start here:- Track your symptoms for a week. Note when they happen, how long they last, and what triggers them.
- Visit the Anxiety and Depression Association of America’s website (ADAA.org) for free screening tools and therapist directories.
- Ask your primary care doctor for a referral to a therapist who specializes in anxiety disorders. Don’t settle for someone who doesn’t mention CBT or exposure therapy.
- If medication is suggested, ask: “Which one? Why? What are the side effects? How long until I feel results?”
- Try one CBT-based app for 30 days. Even 10 minutes a day can make a difference.
Anxiety doesn’t define you. It’s a condition you can learn to manage-with the right tools, support, and time. You don’t have to live in fear. Help is available. And it works.


Emily P
December 19, 2025 AT 00:28I’ve been tracking my panic attacks for a week now. Turns out they hit hardest when I’m scrolling at 2am. No idea why. But writing it down made it feel less like my brain is broken and more like a pattern I can tweak.
Also, the breathing thing? I tried the 4-2-6 method yesterday. Didn’t fix everything. But for the first time in months, I didn’t feel like I was drowning.
Takeysha Turnquest
December 19, 2025 AT 09:17anxiety is just the soul screaming because the world won’t stop spinning
they give you meds to mute the scream but never teach you why it started
we treat symptoms like bugs not wounds
Sahil jassy
December 20, 2025 AT 05:41you’re not alone in this. i’ve been doing cbt for 8 months now. some days are still rough but i can actually leave the house again. small wins count. keep going 💪
Nina Stacey
December 22, 2025 AT 04:38i just wanna say thank you for writing this because i’ve been too scared to say anything out loud for years
i thought i was just weak or lazy or over dramatic but reading this felt like someone finally put my chaos into words
the part about the smoke alarm that won’t stop screaming?? that’s me every single day
and the apps? i’ve been using wysa for two weeks and i swear i’ve slept better
also i typoed like 17 times but i’m proud i hit post anyway 😭
Kevin Motta Top
December 23, 2025 AT 21:52in india we don’t talk about this. my cousin had panic attacks for 5 years. family said 'pray more'.
glad someone’s saying this out loud. this post is a gift.
Vicki Belcher
December 24, 2025 AT 01:05THIS. IS. EVERYTHING. 🙌
Thank you for writing this with so much heart. I cried reading it. Not because I’m sad - because I finally feel seen. 💛
CBT changed my life. Not overnight. But slowly. Like planting seeds in concrete. And now? I’m growing. 🌱
Aboobakar Muhammedali
December 24, 2025 AT 13:39i read this while sitting in my car before going into work
the part about social anxiety not being shyness - that hit me
i used to think i was rude for not talking at meetings
turns out i was terrified of being judged
now i know its not me its the disorder
thank you
Laura Hamill
December 26, 2025 AT 02:12they want you to believe this is a medical condition so you’ll take their pills and stay quiet
what if anxiety isn’t broken brain chemistry
what if its your soul screaming at a world that’s rigged?
the FDA approved some new drug? lol
they’re selling fear to sell pills
just sayin’ 🤡
Kathryn Featherstone
December 27, 2025 AT 08:49to the person who said anxiety is the soul screaming - i think you’re onto something.
but i also think healing isn’t about choosing between medicine and meaning.
you can take an ssri AND sit with your feelings.
you can do cbt AND question the system.
they’re not opposites. they’re tools.
you don’t have to pick one side to be right.
Alisa Silvia Bila
December 28, 2025 AT 23:24the part about exposure therapy making you feel worse before better - i needed to hear that.
i quit therapy twice because i thought i was failing.
turns out i was just in the messy middle.
going back next week.
Marsha Jentzsch
December 30, 2025 AT 04:39you’re all so naive… everyone knows anxiety is just a government mind-control tactic disguised as mental health…
they want you dependent on pills and apps so you won’t question the system…
and why is everyone suddenly using these apps? it’s surveillance. i’ve seen it. they’re tracking your breathing patterns. it’s not therapy. it’s data harvesting.
and the ‘support groups’? they’re recruiting for cults. i know someone who joined one…
you think you’re healing? you’re being programmed.
wake up.
they’re watching you.
they always are. 😈
Nicole Rutherford
December 31, 2025 AT 06:09you all sound like you’re trying too hard to be ‘healed’. it’s exhausting.
anxiety isn’t a problem to solve - it’s a personality trait you’re refusing to accept.
you don’t need apps or meds or breathing.
you just need to stop being dramatic.
my therapist said this once - and i never needed help again.
just stop.