Side Effect Reduction Calculator
Select a condition and treatment type to see results
For years, doctors reached for higher doses of a single drug when a patient’s condition didn’t improve. But what if the real problem wasn’t the dose - but the drug itself? Combination therapy flips that script. Instead of pushing one medication to its limit, it uses two or more at lower doses, working together to get the job done with fewer side effects. This isn’t experimental. It’s now standard practice for high-risk hypertension, type 2 diabetes, and even certain cancers - backed by decades of clinical data and real-world outcomes.
Why Lower Doses Work Better Than High Doses
Think of your body like a machine with limits. Push one part too hard, and it breaks down. That’s what happens with high-dose monotherapy. Take blood pressure meds: a full dose of an ACE inhibitor might lower pressure, but it also triggers a dry cough in nearly 10% of users. A full dose of a calcium channel blocker can cause swollen ankles in 14%. Now, combine half-doses of both. The result? Better pressure control, and those side effects drop by more than half. This isn’t magic. It’s pharmacology. Different drugs hit different targets. One relaxes blood vessels, another helps the kidneys flush out salt. Together, they cover more ground without overloading any single system. A 2024 meta-analysis in Nature Reviews Drug Discovery reviewed 237 trials and found combination therapy delivered 28-42% better results than high-dose single drugs - while cutting side effects by 19-33%.Real-World Examples Across Conditions
In hypertension, the 2023 European Society of Cardiology guidelines recommend starting with a combination of an ACE inhibitor and a calcium channel blocker at half-strength. Patients on this combo saw systolic blood pressure drop 8.7 mmHg more than those on maximum single-drug doses. At the same time, ankle swelling dropped from 14.3% to 4.1%, and cough went from 9.8% to just 2.3%. For type 2 diabetes, metformin alone at 2,000 mg a day can cause nausea and diarrhea in over a quarter of patients. But combine it with a lower dose of an SGLT2 inhibitor - say, 10 mg - and you get the same HbA1c reduction, but gastrointestinal side effects drop to under 12%. Even better: the risk of lactic acidosis, a rare but dangerous complication, nearly disappears. In cancer, it’s even more critical. A full dose of anthracycline can damage the heart. But pair it with a lower dose of cyclophosphamide, and you get the same tumor shrinkage - with half the risk of severe neutropenia and less than a third of the long-term heart damage. The NCCN guidelines now list these combinations as standard for many solid tumors.The Power of the Single Pill
Taking four different pills every day is hard. Taking one pill that contains all four is easier. That’s the idea behind fixed-dose combinations (FDCs). The 2021 Lancet UMPIRE trial gave 12,200 people without heart disease a single pill with aspirin, simvastatin, lisinopril, and atenolol - all at 50-75% of standard doses. Five years later, they had 53% fewer heart attacks, 51% fewer strokes, and 49% lower cardiovascular death rates than those on usual care. Adherence skyrockets with FDCs. The American Heart Association found 68% of patients stuck with single-pill combinations, compared to just 52% on multiple separate pills. Why? Simple: “Easier to remember,” said 74% of users in a survey of 8,432 people. For someone managing high blood pressure, diabetes, and high cholesterol, cutting from six pills down to two or three makes a huge difference.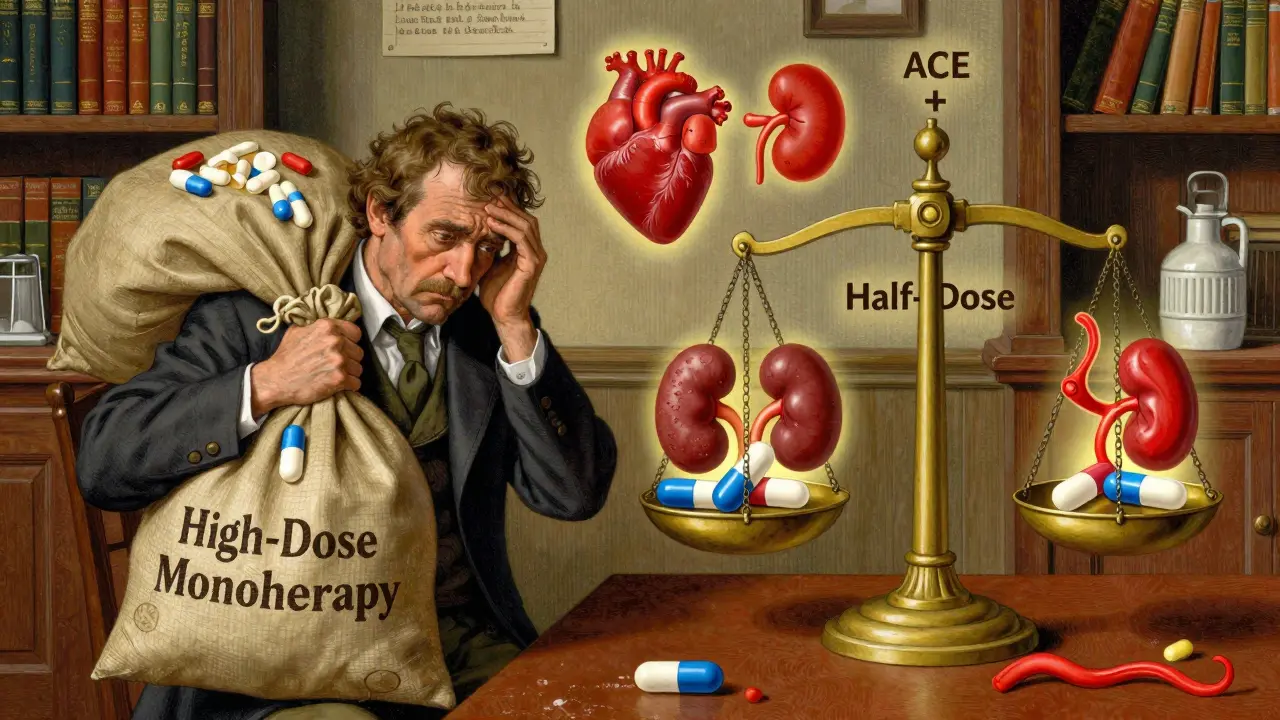
When It Doesn’t Work - and Why
Combination therapy isn’t a silver bullet. A 2022 NEJM study found triple-drug combinations increased the risk of acute kidney injury by 1.8 times in older adults with already reduced kidney function. The FDA’s adverse event database recorded over 2,300 combination-related complications in 2023 - nearly half involved drug interactions in patients over 65 taking five or more meds. And then there’s the cost. A combination therapy averages $4,217 a year, compared to $2,864 for a single drug. But here’s the catch: those extra costs are often offset. In diabetes, the ADA found combination therapy saved $7,842 per patient annually in avoided complications like kidney failure and amputations. Even more troubling: some cancer drug combos don’t work together at all. A 2023 Cell study found 38% of FDA-approved cancer combinations showed no real synergy - meaning patients got more side effects without better results. That’s not innovation. That’s guesswork.Who Should Avoid It?
Not everyone benefits. Older adults with multiple chronic conditions, especially those with kidney problems or on more than five medications, face higher risks. The 2023 ACC Expert Consensus warns that combination therapy increases non-adherence by 27% in patients managing complex regimens. And while FDCs help, they’re not always customizable. If you need to tweak one drug’s dose independently, a combo pill won’t let you. Patients who’ve had bad reactions to any component in the combo should avoid it. And if you’re on blood thinners, certain antibiotics, or supplements like St. John’s wort, your pharmacist needs to check for interactions before you start.
How It’s Changing Treatment
The field is evolving fast. The American Heart Association now recommends starting with four drugs at ultra-low doses for high-risk hypertension patients. The POLYDELPHI trial, enrolling 15,000 people, is testing whether five drugs at just 20-30% of normal doses can slash cardiovascular risk by 70%. Harvard researchers are pushing toward “response-adaptive sequencing” - starting with one combo, then switching or dropping drugs based on how your body responds. This could cut unnecessary drug exposure by 40% while keeping effectiveness. Meanwhile, global adoption is accelerating. In India, polypill use jumped from 5.3% to 18.7% of cardiovascular prescriptions between 2020 and 2023. The FDA approved 47 new combination drugs in 2023 - up from 32 the year before.What to Ask Your Doctor
If you’re on multiple meds or struggling with side effects, ask:- Is there a fixed-dose combo that could replace my current pills?
- Could lowering the dose of one drug and adding another reduce my side effects?
- Am I on any combinations that haven’t been proven to work together?
- Would a pharmacist review help me spot potential interactions?
Bottom Line
Combination therapy at lower doses isn’t about cutting corners. It’s about working smarter. It’s how you get better results with less harm. For millions with chronic conditions, it’s already the gold standard. The real question isn’t whether you should try it - it’s why you haven’t asked about it yet.Is combination therapy safe for older adults?
It can be, but it requires caution. Older adults, especially those with kidney issues or taking five or more medications, face higher risks of drug interactions and acute kidney injury. Always start with low doses, monitor kidney function regularly, and avoid triple combinations unless absolutely necessary. A pharmacist review can help identify hidden risks.
Do combination pills cost more than taking separate drugs?
Yes, the upfront cost is usually higher - often $1,000-$1,500 more per year. But many insurance plans cover FDCs well, and the long-term savings from fewer hospital visits, ER trips, and complications often outweigh the extra cost. In diabetes, for example, combination therapy saves nearly $8,000 per patient annually in avoided complications.
Can I switch from a high-dose single drug to a combination?
Yes - and many patients should. If you’re experiencing side effects or your condition isn’t well-controlled, ask your doctor about switching. Most combinations can be started gradually, often replacing one drug at a time. Never stop or change your meds without medical supervision.
Are there any over-the-counter combination therapies?
There are very few. Some OTC pain relievers combine acetaminophen and caffeine, or aspirin and antacids. But for chronic conditions like high blood pressure or diabetes, all combination therapies are prescription-only. Be wary of supplements marketed as “natural combos” - they’re not regulated and may interact dangerously with your meds.
How long does it take to see results with combination therapy?
It varies. For blood pressure, most patients see improvement within 2-4 weeks. For diabetes, HbA1c levels typically drop noticeably in 8-12 weeks. Cancer treatments may show tumor response in 6-12 weeks. Your doctor will schedule follow-up tests to track progress and adjust doses as needed.
What if I miss a dose of my combination pill?
If you miss one dose, take it as soon as you remember - unless it’s almost time for your next dose. Then skip the missed one and go back to your regular schedule. Never double up. Missing doses can reduce effectiveness and increase the risk of complications. Setting phone reminders or using a pill organizer helps a lot.
Can combination therapy help me reduce my pill burden?
Absolutely. That’s one of its biggest benefits. A single-pill combination can replace two, three, or even four separate pills. For someone taking 8-10 medications a day, switching to a few FDCs can cut their daily pill count in half - making it easier to stick with treatment and reducing confusion.

Peter Sharplin
January 25, 2026 AT 09:59Been on a combo for hypertension for 3 years now. Half-dose lisinopril + half-dose amlodipine. No cough, no swollen ankles, and my BP’s been stable as hell. The only downside? My pharmacy keeps trying to switch me to the brand-name combo pill because it’s ‘more convenient.’ I don’t care about convenient-I care about cost. Generic half-doses still save me $80 a month.
Also, side note: if your doc pushes a full-dose single drug first, ask them why. The guidelines changed five years ago. They might just be lazy.
shivam utkresth
January 27, 2026 AT 01:57Bro in India, we’ve been doing polypills since 2018. My uncle took a 4-drug combo for BP + cholesterol and now he walks 5km daily. No more dizziness. No more ‘doctor, I can’t afford 5 different pills.’ The government even subsidizes it now. But yeah, some rural clinics still give monotherapy because they don’t have the combo stock. It’s not about science here-it’s about supply chains.
Also, the FDA approved 47 new combos last year? We’ve got 120+ in the public health system. We don’t wait for approval-we adapt. Real people need real solutions, not red tape.
John Wippler
January 27, 2026 AT 02:38This isn’t just pharmacology. It’s humility. We used to think more was better. Stronger. Bigger. But the body isn’t a car you can just rev higher. It’s a symphony. One instrument too loud, and the whole thing falls apart.
Combination therapy is the medical version of ‘less is more.’ It’s the quiet genius of working with the system instead of smashing it. We’ve spent decades trying to force biology into our ego-driven models. Now we’re finally listening.
And honestly? The fact that patients stick with FDCs better? That’s not about pills. That’s about dignity. People don’t fail treatment. Treatment fails people when it’s too complicated, too expensive, too punishing.
Let’s stop calling it ‘therapy.’ Let’s call it respect.
Aurelie L.
January 28, 2026 AT 05:27My mom died from a combo reaction. She was on 7 meds. They added a new one without checking interactions. She went into renal failure in 72 hours. This isn’t ‘smart medicine.’ It’s a lottery with your life.
Stop glorifying this.
Joanna Domżalska
January 29, 2026 AT 05:55So you’re telling me if I take 1/4 of four drugs, I get the same effect as one full dose? That’s not science. That’s math magic. Where’s the clinical trial proving that 1/4 of drug A + 1/4 of drug B + 1/4 of drug C + 1/4 of drug D equals 1 full dose of one? It doesn’t work that way.
Also, the ‘FDA approved 47 combos’ thing? That’s not progress. That’s pharma’s way of patenting old drugs in new packaging. Look at the prices. They’re higher. Always higher.
And don’t get me started on the ‘polypill’ hype. You think people in rural India are taking it because it’s better? Or because they have no other option?
This isn’t innovation. It’s corporate rebranding with a side of virtue signaling.
Ashley Porter
January 30, 2026 AT 08:32Just got prescribed a combo for my type 2. Metformin + semaglutide at low dose. Zero nausea. Lost 12 lbs in 6 weeks. My A1c dropped from 8.1 to 6.4. Doc said this combo’s been in trials since 2020. Why wasn’t I on it sooner?
Also, the pill’s tiny. Like, palm-sized. I feel like I’m cheating.
Kipper Pickens
February 1, 2026 AT 08:30Let’s not forget the pharmacokinetics. Lower doses reduce CYP450 saturation, which means fewer drug-drug interactions. That’s why combo therapy works-not just additive effects, but reduced metabolic burden. The liver doesn’t get overwhelmed. The kidneys don’t get clogged. The GI tract doesn’t revolt.
It’s not magic. It’s systems biology. And the data’s solid. The 2024 Nature meta-analysis? That’s not cherry-picked. That’s the entire literature.
Also, FDCs reduce pill burden → better adherence → lower hospitalization rates → lower overall cost. Even if the sticker price is higher, the system saves money. That’s not marketing. That’s health economics 101.
Faisal Mohamed
February 2, 2026 AT 15:12Bro I’ve been on a combo for 2 years and I’m basically a new person 😭
Used to be a zombie at 3pm. Now I run. My doc said ‘try this’ and I was like ‘nah’ but then I did and now I’m like… why did no one tell me this was a thing?
Also the pill looks like a Skittle. I’m lowkey obsessed.
PS: my grandma took the same combo and now she’s dancing at weddings again 💃🕺
rasna saha
February 3, 2026 AT 07:04I’m a nurse in rural India. We hand out polypills to patients who can’t afford to come back every month. One pill. One dose. One chance. I’ve seen men who couldn’t walk 10 steps start riding bikes again. No fancy lab tests. No insurance. Just a simple combo.
This isn’t about tech. It’s about access. If we wait for perfect trials, people die waiting. Sometimes the best medicine is the one you can actually take.
Skye Kooyman
February 3, 2026 AT 08:29James Nicoll
February 4, 2026 AT 11:01So the medical establishment finally figured out that less can be more? Took ‘em long enough. We’ve known since the 70s that high-dose monotherapy is just ego-driven medicine. But hey, at least now the journals have catchphrases for it.
‘Combination therapy’ sounds fancy. ‘Don’t overdose your patients’ sounds like common sense. Guess which one gets published?
Also, the polypill? That’s not innovation. That’s capitalism repackaging the same shit with a new label and a 200% markup. But hey, if it gets people to take their meds, I’ll take it. Just don’t call it a breakthrough. Call it a correction.
Uche Okoro
February 4, 2026 AT 23:15Let’s be precise. The 2023 NEJM study cited a 1.8-fold increase in acute kidney injury among elderly polypharmacy patients. Not ‘some risk.’ Not ‘possible.’ 1.8-fold. That’s statistically significant. p < 0.001.
And the FDA adverse event database? 2,300 incidents. 47% involved patients on ≥5 medications. That’s not anecdotal. That’s population-level data.
Combination therapy is not universally beneficial. It is context-dependent. To present it as a panacea is not just misleading-it’s dangerous. The evidence is nuanced. The narrative shouldn’t be.
Marie-Pier D.
February 6, 2026 AT 11:34My sister has lupus and was on high-dose prednisone for years. Horrible side effects-moon face, insomnia, anxiety. They switched her to a combo with hydroxychloroquine + low-dose azathioprine. She’s got her energy back. Her skin looks normal. She’s not crying every night.
I cried when I saw her smile again. This isn’t just science. This is someone’s life being given back.
Thank you for writing this. I’m printing it out for her doctor.