- 12
Acid Medication Risk Calculator
This tool helps you understand the potential risks of taking both H2 blockers (like famotidine) and PPIs (like omeprazole) together. Based on clinical evidence, this combination is rarely necessary and increases your risk of serious complications without significant benefits.
Your Medication Details
Risk Assessment Results
Many people take acid-suppressing medications without realizing they might be on more than they need. It’s common to see prescriptions for both an H2 blocker and a proton pump inhibitor (PPI) together-especially in hospitals or for chronic heartburn. But here’s the truth: combining H2 blockers and PPIs is rarely necessary, and often risky. For most people, one of these drugs is enough. Adding the other doesn’t improve symptoms-it just adds side effects, costs, and complications.
How H2 Blockers and PPIs Actually Work
H2 blockers like famotidine (Pepcid) and cimetidine (Tagamet) reduce stomach acid by blocking histamine from telling your stomach cells to make more acid. They start working within an hour and last 6 to 12 hours. They’re good for quick relief, especially if you’re having a flare-up after a big meal.
PPIs like omeprazole (Prilosec) and esomeprazole (Nexium) work differently. They shut down the actual acid-producing pumps in your stomach lining. This is a deeper, longer-lasting effect-up to 90-98% reduction in acid. But they don’t work right away. It takes 2 to 5 days to reach full strength. That’s why people often feel worse before they feel better when starting a PPI.
Here’s the problem: PPIs suppress acid so completely that there’s almost no histamine left to stimulate the stomach. That means H2 blockers lose their target. Studies show adding an H2 blocker to a PPI gives you maybe a 5% extra drop in acid-barely noticeable, and never enough to improve symptoms like heartburn or healing of the esophagus.
Why Doctors Still Prescribe Both (And Why They Shouldn’t)
Many doctors still prescribe both because they think, “More acid suppression = better.” But that’s outdated thinking. The American College of Gastroenterology reviewed 12 clinical trials with nearly 3,000 patients and found no benefit from combining the two for GERD. The same goes for the American Gastroenterological Association-they explicitly say: don’t do it routinely.
The real reason this combo persists? Habit. Tradition. And sometimes, patient pressure. People hear “stronger medication = better,” and ask for it. Doctors, wanting to please, prescribe it-without checking if it’s needed.
There’s one narrow exception: documented nocturnal acid breakthrough. That means your stomach pH drops below 4 for more than an hour between midnight and 6 a.m., even while taking a twice-daily PPI. This is rare. It’s confirmed with a 24-hour pH test, not guesswork. Even then, the H2 blocker should be temporary-used for 4 to 8 weeks, then stopped. If symptoms don’t improve, it’s not helping.
The Hidden Dangers of Combining These Drugs
It’s not just useless-it’s dangerous. Studies tracking tens of thousands of patients show PPIs alone carry risks. Add an H2 blocker, and you’re doubling exposure to those problems.
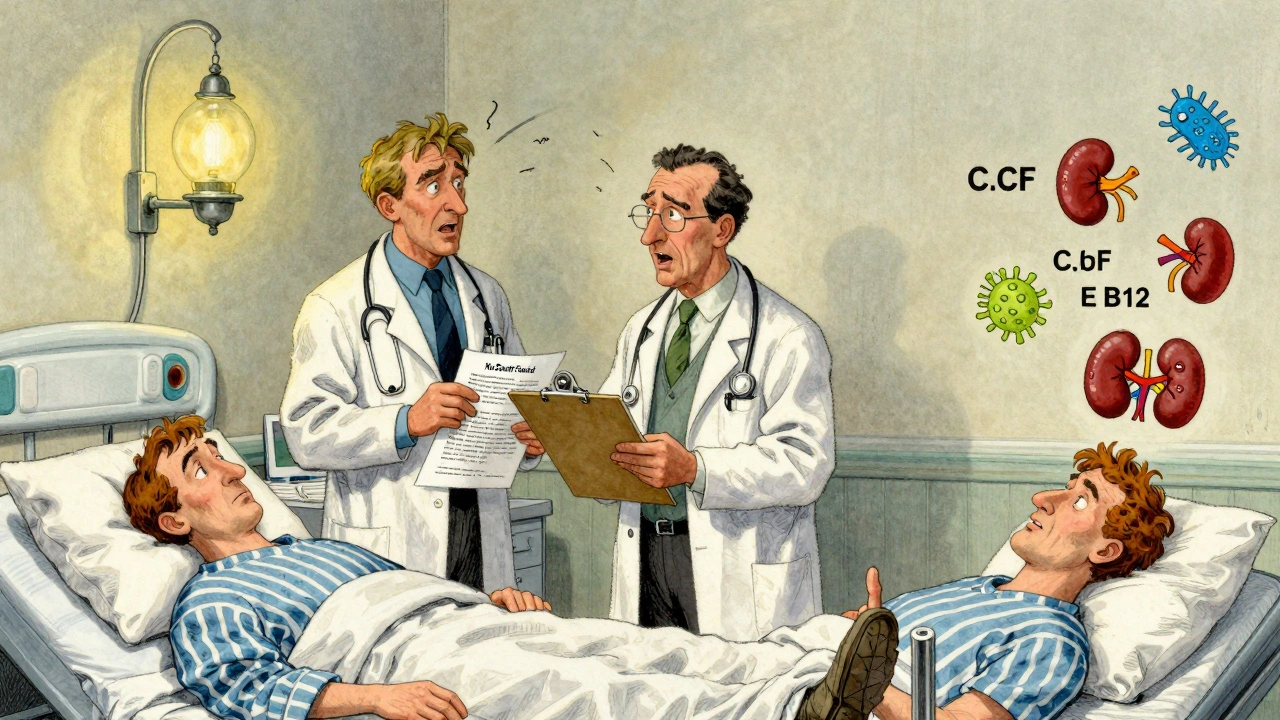
One major risk: pneumonia. In ICU patients, those on PPIs had a 30% higher chance of getting hospital-acquired pneumonia than those on H2 blockers. Why? Less stomach acid means more bacteria survive and travel up into the lungs.
Clostridium difficile (C. diff) infection risk jumps 32% with PPIs. This isn’t just diarrhea-it can be life-threatening, especially in older adults. H2 blockers don’t carry the same level of risk.
Then there’s kidney damage. A 2021 study of over 3,600 people with chronic kidney disease found those on PPIs were 28% more likely to progress to kidney failure than those on H2 blockers. The longer you’re on a PPI, the higher the risk.
And bone fractures. The FDA warned in 2014 that long-term, high-dose PPI use increases fracture risk, likely because acid suppression interferes with calcium absorption. H2 blockers don’t show the same pattern.
Even vitamin deficiencies are more common with PPIs. Low B12, magnesium, and iron levels show up more often in long-term users. H2 blockers are much less likely to cause this.
What Patients Are Saying
On Drugs.com, 68% of users taking PPIs reported side effects-headaches, diarrhea, bloating, fatigue. On Reddit’s r/GERD community, 42% of users say they can’t stop PPIs without rebound heartburn. That’s not addiction-it’s physiological rebound. Your stomach overproduces acid after months of suppression. Suddenly stopping the PPI feels like a firestorm.
Worse, many don’t even know why they’re on both drugs. A survey by the American College of Gastroenterology found 31% of patients on combination therapy couldn’t explain why. 64% didn’t know the risks. That’s not informed consent. That’s negligence.

What You Should Do Instead
If you’re on both, ask your doctor this: “Why am I on two acid blockers? Is there proof I need both?”
Here’s a better path:
- Start with the lowest effective dose of a PPI-once daily, not twice.
- Give it 4 weeks to work. Most people improve with this alone.
- If symptoms return, don’t add an H2 blocker. Look at diet, weight, timing of meals, or possible hiatal hernia.
- Only consider an H2 blocker at night if you have confirmed nocturnal breakthrough-confirmed by a pH test.
- Plan a “PPI time-out” every 90 days. Try stopping it for 2 weeks. If symptoms don’t come back, you don’t need it.
Many people who think they need lifelong acid suppression don’t. Lifestyle changes-avoiding late meals, cutting back on caffeine and alcohol, losing weight, elevating the head of the bed-often fix the problem without drugs at all.
The Bigger Picture
This isn’t just about one drug combo. It’s about how medicine overuses medications. The U.S. spends $12.3 billion a year on acid-suppressing drugs. PPIs make up 78% of prescriptions. Yet studies show up to 70% of PPI prescriptions are inappropriate. Add H2 blockers to that, and you’ve got a $1.5 billion waste problem.
Hospitals are now being penalized if more than 15% of their patients get both drugs without proper documentation. That’s because the data is clear: this combo rarely helps, and often harms.
The future? Precision medicine. Researchers are looking for genetic markers that might predict who actually benefits from combination therapy. But right now, we don’t have those tools. So the safest rule is simple: if you don’t have proof you need both, you probably don’t.
Less is more when it comes to acid suppression. Your stomach needs acid to digest food, kill bacteria, and absorb nutrients. Turning it off completely isn’t health-it’s a medical intervention. And like any intervention, it should be used only when necessary, and stopped when it’s no longer helping.

Lydia Zhang
December 2, 2025 AT 06:16Been on PPI for 3 years. Stopped last month. No rebound. My stomach didn’t explode. Weird.
Kay Lam
December 3, 2025 AT 22:52I get why doctors do this. They’re trained to treat symptoms, not root causes. If you’re in a 15-minute appointment and someone says ‘my chest burns,’ the easiest thing is to write a script. No one has time to ask about sleep posture or whether you eat pizza at midnight. But that’s not medicine. That’s damage control. We’ve turned a biological system into a broken faucet that needs constant duct tape. Acid isn’t the enemy. Lifestyle is. And yet we keep prescribing more drugs instead of asking people to change their habits. It’s easier for everyone. Until you’re on five meds and your kidneys are failing and you don’t even know why you started taking any of them in the first place.
Shashank Vira
December 4, 2025 AT 03:08How tragic that the medical-industrial complex has reduced human physiology to a chemical equation. The stomach is not a malfunctioning boiler. It is a finely tuned ecosystem, honed over millennia, and we, with our pharmacological hubris, believe we can silence its roar with a pill. To combine H2 blockers with PPIs is not therapy-it is ontological arrogance. The body does not need to be silenced. It needs to be listened to. And yet, we deafen it with proton pumps and histamine blockers, then wonder why it screams back with C. diff and osteoporosis.
Irving Steinberg
December 4, 2025 AT 23:16Yessss this is so true 😌 I was on both for 2 years and just dropped the H2 blocker last week. No drama. No firestorm. Just… normal digestion. Why do we make everything so complicated??
Courtney Co
December 6, 2025 AT 08:11But what if you’re a single mom working two jobs and you can’t afford to eat at 5pm or sleep with your head elevated? What if your doctor says ‘just take both’ and you’re too tired to argue? Who’s responsible then? The system? The doctor? The patient? I just want to sleep without my throat feeling like it’s on fire. Is that too much to ask?
Adrian Barnes
December 8, 2025 AT 01:09It is imperative to underscore that the concomitant administration of H2 receptor antagonists and proton pump inhibitors constitutes a clinically indefensible practice in the absence of validated physiological indicators. The literature is unequivocal: no therapeutic benefit accrues from such dual suppression, while the risk profile escalates significantly across multiple organ systems. This is not merely suboptimal care-it is a systemic failure of evidence-based practice. The persistence of this paradigm reflects a disturbing epistemic decay within clinical medicine.
Jaswinder Singh
December 9, 2025 AT 17:11Bro you’re right but you’re also talking to people who don’t even know what ‘GERD’ stands for. Most of us just know our chest hurts and we don’t want to feel like we swallowed a hot coal. I got off both after 6 months of eating like a monk and sleeping on a brick. But telling someone to ‘just change their lifestyle’ when they’re working 80 hours a week and eating gas station food? That’s not advice. That’s a middle finger.
Bee Floyd
December 10, 2025 AT 03:13There’s something poetic about how we treat stomach acid like a villain. It’s not evil. It’s doing its job. We’ve turned digestion into a war we’re winning with chemicals, but losing in every other way. I used to think I needed PPIs forever. Then I started walking after dinner. Not because I read a study. Because my grandma did it. And guess what? The fire went out. No pills. Just time. And patience. And maybe a little respect for the body that’s been carrying us all along.
Jeremy Butler
December 10, 2025 AT 13:31The ontological implications of pharmacological overreach in gastroenterology reveal a deeper epistemological crisis: the substitution of mechanistic intervention for holistic understanding. The reduction of gastric physiology to a binary of acid/no acid reflects a Cartesian fragmentation of the body that ignores the interoceptive, neural, and microbiological feedback loops governing digestion. The prescription of dual suppression is not merely inappropriate-it is a symptom of a medical culture that has abandoned phenomenological inquiry in favor of algorithmic treatment.
Eric Vlach
December 10, 2025 AT 15:39I used to be the guy who asked for both because I thought stronger = better. Then I got sick from C. diff and spent a week in the hospital. Now I tell everyone: if you’re on two, ask why. And if they can’t give you a good answer, ask for a second opinion. Seriously. Your gut doesn’t need a sledgehammer. It needs a key.
Souvik Datta
December 12, 2025 AT 04:37Let me tell you something from the other side of the world. In India, we’ve always known that food timing matters. Eat early. Don’t lie down after. Chai after dinner? No. Spicy food at midnight? No. We didn’t need PPIs until we started copying Western habits. Now we’re copying Western prescriptions too. But the body doesn’t care about your country. It only cares about what you put in it and when. Stop blaming the medicine. Start blaming the schedule.
Priyam Tomar
December 12, 2025 AT 05:15Actually, you’re all wrong. The real issue is that PPIs are overprescribed because they’re profitable. But H2 blockers? They’re generics. Cheap. Safe. And if you’re still having symptoms on a PPI, adding an H2 blocker at night isn’t dumb-it’s smart. The studies you cite? They’re funded by pharma trying to kill off the H2 market. Wake up. Sometimes two drugs work better. Not always. But sometimes. Don’t throw the baby out with the bathwater.