Drug Interaction Risk Calculator
Assess Your Medication Risk
This tool estimates your risk of adverse drug reactions based on your health conditions and medications. The article explains why comorbidities increase drug side effects by altering how your body processes medications.
When you’re taking medication, you expect it to help. But if you have other health conditions, the risks can change dramatically. A drug that’s safe for one person might cause serious side effects in another - not because of the medicine itself, but because of what else is going on in the body. This isn’t rare. It’s the new normal. More than two out of every three adults over 65 have at least two chronic conditions. And for them, every pill carries a hidden danger.
Why Existing Conditions Make Drugs More Dangerous
Your body doesn’t process drugs the same way when you have liver disease, kidney problems, heart failure, or diabetes. These conditions change how your body absorbs, breaks down, and gets rid of medications. For example, liver disease can cut the activity of key enzymes by 30% to 50%. That means drugs like statins, antidepressants, or painkillers stay in your system longer than they should. The result? Higher doses than intended, leading to dizziness, confusion, or even falls. Kidney impairment does something similar. If your kidneys aren’t filtering well, drugs that are cleared through urine - like certain antibiotics, blood pressure meds, or diabetes pills - build up. This isn’t theoretical. Studies show patients with reduced kidney function are up to four times more likely to suffer serious side effects from these drugs. Then there’s the body’s sensitivity. Someone with Parkinson’s might react badly to antipsychotics because their brain is already struggling with movement control. A person with heart disease might have a dangerous spike in blood pressure from a decongestant. These aren’t just side effects - they’re disease-drug interactions. And they’re often missed because clinical trials rarely include people with multiple conditions.The Polypharmacy Trap
Most people with comorbidities aren’t taking one drug. They’re taking five, six, or more. The average elderly patient with multiple chronic conditions takes 4.3 medications daily. Nearly half take five or more. That’s not just inconvenient - it’s a minefield. Each new drug adds more chances for interactions. One drug might slow down how another is broken down. Another might compete for the same liver enzyme. In cancer patients, studies found that 65 out of 100 had dangerous drug combinations. About one-third of those were major - meaning they could cause permanent harm or death. The numbers are brutal. Patients with three or more chronic conditions are 2.5 times more likely to be hospitalized because of a drug reaction. And the symptoms? They’re not always obvious. Weakness shows up in 36% of cases. Dizziness? 12%. Headaches, nausea, vomiting, insomnia - these aren’t just annoyances. They’re warning signs that your body can’t handle the mix.Who’s Most at Risk?
It’s not just older adults. People with substance use disorders are at high risk too. Nearly 80% of those in treatment for alcohol or opioids also smoke. That means their liver is already under stress, and many of the drugs they take - including painkillers or mental health meds - are processed by the same system. The risk of overdose or liver damage skyrockets. Chronic pain patients are another high-risk group. Around 10% end up misusing their own prescription opioids. That’s not just addiction - it’s a cycle. The pain leads to more drugs, which cause side effects, which lead to more meds to treat those side effects. It’s a spiral. Women over 75 are especially vulnerable. Studies show they’re almost three times more likely to be prescribed medications that are considered unsafe for older adults - things like certain sleeping pills, antihistamines, or muscle relaxants. These drugs can cause confusion, falls, or even hip fractures.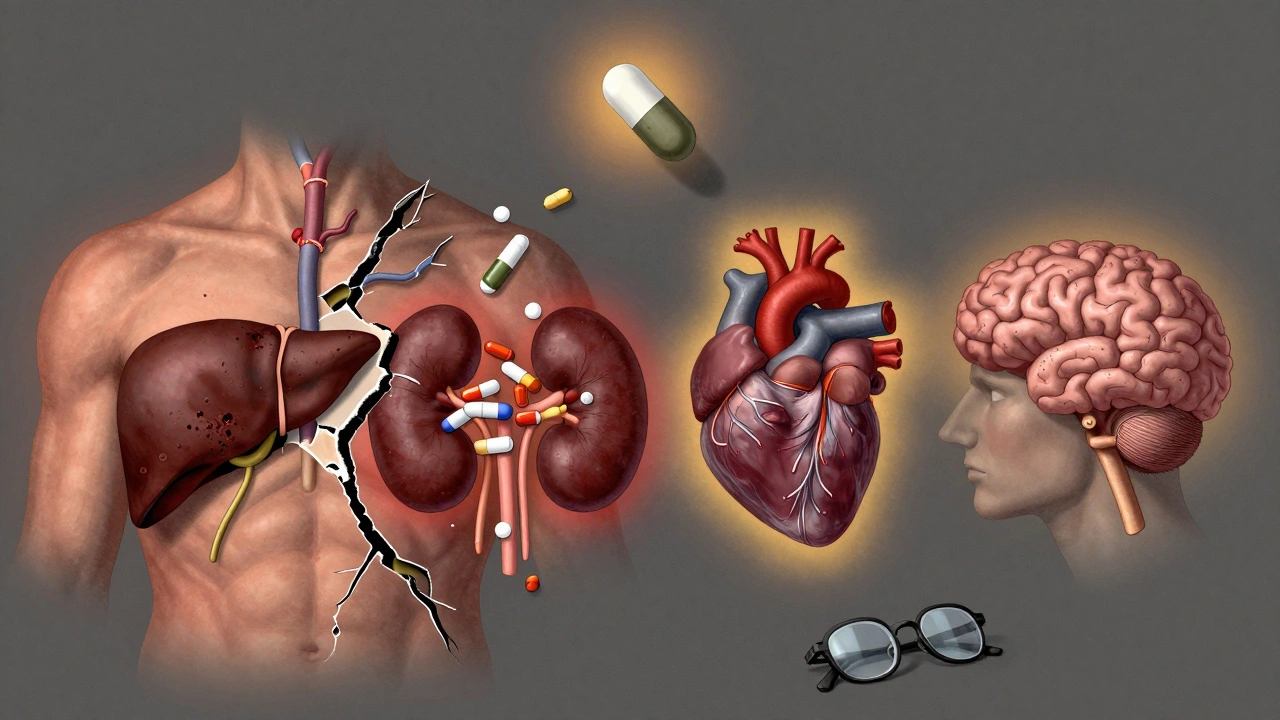
What Happens in the Real World?
Doctors don’t always see the full picture. A patient might see a cardiologist, a rheumatologist, a neurologist, and a primary care doctor - all prescribing without knowing what the others have ordered. Sixty-eight percent of people with three or more conditions see five or more specialists. That’s a recipe for disaster. In one study, 46% of older patients were given at least one medication that shouldn’t have been prescribed to them based on established safety guidelines. These are called Potentially Inappropriate Medications (PIMs). And they’re not harmless. They contribute to 40% to 60% of all medication problems in elderly primary care patients. The cost? It’s not just physical. In cancer care, preventable drug interactions add $1,200 to $2,500 per incident in extra hospital bills. And that’s just one slice of the problem.How to Protect Yourself
The good news? There are ways to reduce the risk. Start with a full medication review. Not just a quick check - a deep dive. Clinical pharmacists who specialize in this have reduced adverse reactions by 22% in patients with multiple conditions. They look at every pill, supplement, and over-the-counter drug. They ask: Is this still needed? Could it interact with another? Is there a safer alternative? Ask your doctor about the STOPP/START criteria. These are evidence-based tools that help identify which drugs to stop and which to start. They’re not magic, but they’ve cut hospitalizations from drug reactions by 17% in older patients. Use technology. Electronic health records with built-in comorbidity alerts are now common. They flag when a new prescription might clash with a patient’s existing conditions. One study showed a 35% drop in unsafe prescribing when these tools were used. Keep a written list. Not just the names - include doses and why you’re taking each one. Bring it to every appointment. Even if you think your doctor knows your history, they might not. And if you’re seeing multiple specialists, you’re the only one who has the full picture.
The Future Is Personal
New tools are emerging. The NIH launched a database in early 2024 that tracks over 12 million patient records to find hidden drug-comorbidity risks. It’s already identified 217 new dangerous combinations. Machine learning is getting better at predicting who’s at risk. One system correctly flagged 89% of potential adverse reactions based on a patient’s conditions and meds - far better than older methods. And soon, doctors may be able to use genetic testing and real-time lab data to model how your body will handle a drug before you even take it. Early trials show this approach can cut side effects by 40%. The bottom line? Comorbidities aren’t just background noise. They’re a core part of your drug risk profile. Ignoring them isn’t negligence - it’s dangerous. But with the right awareness and tools, you can take control.What You Can Do Today
- Ask your doctor: “Could any of my conditions make my medications more risky?”
- Request a full medication review by a pharmacist - especially if you take five or more drugs.
- Keep a written list of everything you take, including vitamins and supplements.
- Don’t assume your specialists are talking to each other. Be the one who connects the dots.
- If you feel dizzy, weak, or confused after starting a new drug - don’t wait. Call your doctor.
Medications save lives. But they can also harm - especially when your body is already under stress. Knowing how your conditions change your drug risk isn’t optional. It’s essential.
Can comorbidities make side effects worse even if I’m not on many drugs?
Yes. Even a single medication can become risky if you have a condition like liver disease, kidney impairment, or heart failure. These conditions change how your body handles drugs. For example, a standard dose of a painkiller might stay in your system too long if your liver isn’t working well, leading to drowsiness or confusion. You don’t need to be on five drugs to be at risk - just one, combined with a chronic condition, can be enough.
Are over-the-counter drugs safe if I have comorbidities?
Not always. Many OTC meds - like cold medicines with pseudoephedrine, antacids with magnesium, or sleep aids with diphenhydramine - can interact with chronic conditions. For example, decongestants can raise blood pressure in people with heart disease. Sleep aids can worsen confusion in those with dementia. Always check with your pharmacist before taking anything new, even if it’s sold without a prescription.
Why aren’t clinical trials including people with multiple conditions?
Most drug trials exclude patients with multiple chronic diseases because they’re seen as “too complex.” This creates a huge gap. About 70% to 80% of older adults with comorbidities are left out of the studies that determine if a drug is safe. That means we’re often guessing how it will affect real patients - the very people who need it most.
How do I know if a side effect is from a drug or my condition?
Timing matters. If a new symptom started within days or weeks of beginning a new medication, it’s likely drug-related. Common red flags include sudden dizziness, confusion, unexplained fatigue, nausea, or changes in urination. Keep a symptom diary and share it with your doctor. They can compare it to known side effect profiles and check for interactions.
Can I just stop a medication if I think it’s causing problems?
Never stop a medication without talking to your doctor first. Some drugs, like blood pressure or seizure meds, can cause dangerous rebound effects if stopped suddenly. Instead, note your symptoms, bring your full medication list to your next appointment, and ask: “Could this be related to one of my drugs? Is there a safer option?”
What’s the best way to avoid dangerous drug interactions?
Use one pharmacy for all your prescriptions - they can flag interactions across all your meds. Ask for a medication review by a clinical pharmacist. Keep an updated list of everything you take. And always ask: “What happens if I stop this? What happens if I keep it?”

Nancy Carlsen
December 6, 2025 AT 01:58This is so important!! 🙌 I watched my mom go through this last year - started on a new pain med, got dizzy, fell, broke her hip. Turns out her kidney function had dropped and the drug was building up. She’s okay now, but it was terrifying. Please, if you’re on more than 3 meds, get a pharmacist review. It’s free at most pharmacies and could save your life. 💙
Ted Rosenwasser
December 7, 2025 AT 11:41Let’s be real - the medical system is a profit-driven circus. Drug companies fund trials that exclude anyone over 65 or with comorbidities because they don’t want to see side effects. Then they sell the same pills to those exact people anyway. It’s not negligence - it’s calculated exploitation. The FDA is complicit. Wake up.
Helen Maples
December 8, 2025 AT 19:40Stop using emoticons and get serious. This is a life-or-death issue, not a TikTok trend. The data is clear: polypharmacy in patients with three or more chronic conditions increases hospitalization risk by 250%. That’s not a suggestion - it’s a clinical emergency. If you’re not doing a full med review with a clinical pharmacist, you’re gambling with your life. Period.
Ashley Farmer
December 9, 2025 AT 01:42I just want to say - if you’re reading this and feeling overwhelmed, you’re not alone. I’ve been there. My dad was on 8 meds, and we didn’t realize how much they were interacting until he started hallucinating. We got a pharmacist involved, cut three unnecessary ones, and he’s been his old self again. It’s not about taking less - it’s about taking the right things. You’ve got this.
David Brooks
December 10, 2025 AT 15:36Y’ALL. I just had a 78-year-old client who was on 11 meds - including a sleeping pill, a muscle relaxer, and an antihistamine for allergies. She was falling every week. We pulled the whole list, worked with her pharmacist, and got her down to 4 essential meds. She’s hiking again. 🤯 This isn’t just about pills - it’s about freedom. Don’t let Big Pharma steal your mobility.
Jennifer Anderson
December 12, 2025 AT 07:18omg i had no idea otc stuff could be so dangerous 😭 i was taking benadryl for sleep and my knee pain med was making me foggy - turns out both are bad for kidneys. my pharmacist told me to stop and now i feel like a new person. y’all gotta talk to your pharmacist, not just your dr. they know way more than you think!
Sadie Nastor
December 13, 2025 AT 19:08thank you for writing this. i’ve been scared to ask my doctors anything because i don’t want to seem ‘difficult.’ but this post made me realize - i’m not being difficult, i’m being smart. i printed out the list of meds and brought it to my last appointment. my cardiologist actually thanked me. it’s okay to be your own advocate. you’re not bothering anyone.
Nicholas Heer
December 14, 2025 AT 05:04THIS IS A GLOBALIST PHARMA CONSPIRACY. They don’t want you healthy - they want you dependent. The WHO, CDC, and FDA are all in bed with Big Pharma. They exclude elderly patients from trials because they don’t want the truth to get out: most of these drugs are toxic garbage designed to keep you on the hamster wheel. They even suppress studies that show natural alternatives work better. Wake up, sheeple.
Sangram Lavte
December 15, 2025 AT 19:35In India, we call this ‘polypharmacy chaos.’ Many elders here take 6-8 medicines because each specialist gives their own script. No one talks. I saw a man on 11 drugs - including two for high blood pressure that cancel each other out. His family didn’t know. We made a simple list, brought it to his GP, and cut 4. He stopped falling. Simple solutions work. Don’t overcomplicate it.
Oliver Damon
December 16, 2025 AT 22:43There’s an epistemological gap here: clinical guidelines are built on idealized populations, but lived experience is inherently messy. The reductionist model of ‘one disease, one drug’ fails catastrophically in multimorbidity. We need systems thinking in pharmacology - not siloed specialty care. The current paradigm is not just inefficient - it’s ontologically flawed. We must shift from disease-centric to person-centric prescribing.
Kurt Russell
December 17, 2025 AT 09:45LOOK - I used to be a nurse in a geriatric unit. I’ve seen people die from a simple OTC cold med because no one checked their heart meds. This isn’t theory. This is real life. If you’re over 65 and on more than 3 pills - STOP. Right now. Go to your pharmacy. Ask for a med review. Do it today. Your future self will cry tears of joy. I promise.
Stacy here
December 17, 2025 AT 18:20They don’t want you to know this - but the entire pharmaceutical industry is built on keeping you sick. They profit from side effects. That’s why they don’t fund studies on drug interactions in real people. They want you confused, dizzy, falling, and back for more. And they’ve got the FDA, the AMA, and your doctor on their payroll. You’re not a patient - you’re a revenue stream.
Kyle Flores
December 19, 2025 AT 04:47i had no idea my grandma’s confusion was from her zzzquil. she was taking it for sleep, but her kidney’s not great. we switched her to melatonin and she’s been way calmer. i wish i’d known sooner. y’all, just ask your pharmacist - they’re the real heroes. they don’t get enough love.
Ryan Sullivan
December 19, 2025 AT 22:40Pathetic. This is why America is collapsing. You people treat medicine like a buffet. ‘Oh, I’ll just take this pill for this, and that pill for that.’ No wonder your life expectancy is dropping. You don’t need a list - you need discipline. Stop self-medicating. Stop trusting algorithms. Stop being lazy. Fix your lifestyle. Then maybe you won’t need 10 drugs.
Wesley Phillips
December 21, 2025 AT 14:29Bro I got 7 meds and I still run marathons. You’re all overreacting. My doc said I’m fine. If you’re scared of pills, maybe don’t take them. Problem solved. Also - why is everyone so obsessed with ‘reviewing’? Just chill. Life’s too short to be paranoid about Tylenol.
Olivia Hand
December 22, 2025 AT 04:52What’s the actual prevalence of PIMs in primary care? The article says 40-60% of medication problems - but is that per patient or per prescription? And are we controlling for age, socioeconomic status, and access to pharmacy care? I’m skeptical of these stats without context.
Desmond Khoo
December 23, 2025 AT 19:05just started a med review with my pharmacist and holy cow - i was on 2 things i didn’t even need. one was for a rash i had in 2020. 🤦♂️ she also found a bad combo between my blood pressure med and my turmeric supplement. we cut it and i’ve got more energy. best $0 i ever spent.
Louis Llaine
December 24, 2025 AT 23:54Wow. A whole article about pills. Next up: ‘How Breathing Can Make You Sick If You Have Asthma.’ Groundbreaking. I’m sure the FDA is shaking in their boots.
Jane Quitain
December 25, 2025 AT 18:02i was so scared to ask my doctor about my dizziness but then i wrote it down and showed him - turns out it was my new diabetes med. he changed it right away. i feel like a hero for speaking up. you guys are all so brave for sharing your stories. i’m proud of us 💪