Every year, tens of thousands of children in the U.S. end up in emergency rooms after swallowing pills they found at home. Seniors mix up medications because bottles look too similar. Insulin loses potency because it was left on the counter. These aren’t rare accidents-they’re predictable results of poor storage habits. A home medication storage checklist isn’t just a good idea. It’s a lifeline.
Where to Store Medications (And Where Not To)
The bathroom cabinet is the worst place for most medicines. It’s hot, humid, and full of sudden temperature swings. A hot shower can push humidity levels to 90% and raise the cabinet temperature by 15 degrees. That’s enough to break down pills, creams, and inhalers faster than you think. The FDA says some medications lose up to 50% of their strength in just a few months under these conditions. Instead, pick a cool, dry spot away from windows and heat sources. A linen closet, a bedroom drawer, or a low cabinet in a hallway works best. The ideal environment is between 68-77°F (20-25°C) with humidity around 40-50%. Keep it out of direct sunlight too-light can degrade certain drugs. If your medicine comes in a clear bottle, slip it into an opaque container or wrap it in aluminum foil.Lock It Down-Especially If You Have Kids or Teens
Standard medicine cabinets? They’re useless against curious hands. The Consumer Product Safety Commission found they stop only 12% of kids under six from getting into pills. A 2023 Pediatrics study showed households using locked medicine lockboxes had 92% fewer accidental ingestions. Use a lockbox with a combination lock-it’s more reliable than a key. Kids can’t lose a code. Keep it at least four feet off the ground, behind three closed doors if possible. Store all medications, even vitamins and topical creams, in the same locked space. Don’t leave pills on a nightstand, even for a minute. A 2022 study found 70% of childhood poisonings happen when meds are left unattended for less than 10 minutes. If you have teens, know this: 30% of teens who misuse prescription drugs get them from their own home. A locked box isn’t about distrust-it’s about safety. Controlled substances like opioids or strong painkillers need double locking-even if they’re refrigerated.Separate, Label, and Organize
Mixing up medications is one of the leading causes of home errors. One person’s blood pressure pill can look just like another’s anxiety med. The Institute for Safe Medication Practices says separating meds by household member cuts wrong-medication use by 63%. Use separate bins, shelves, or even different drawers. Label each section clearly: “John’s Meds,” “Mary’s Meds.” If you use a pill organizer, keep the original bottles nearby as backup. Never transfer pills to unmarked containers. High-risk meds like insulin, warfarin, or opioids need extra attention. Mark them with bright “High Alert” stickers. Store them separately from everything else. Insulin, for example, must be refrigerated at 36-46°F until opened. Once in use, it’s stable at room temperature for 14 to 56 days, depending on the type. Keep a thermometer inside the fridge and check it daily.
Track Expirations Like a Pro
Most people don’t know how to tell if a pill is still good. You can’t always see it. But 68% of homes have at least one expired medication. The FDA says 82% of pills retain 90% potency one year past expiration-if stored right. But after two years, that drops to 65%. After three? Just 42%. Check every six months. Set a reminder for the same day as daylight saving time changes-spring forward, fall back. That’s when most people remember to reset clocks. Use that moment to sort through meds. Look for signs of degradation: pills that crumble, change color, or smell odd. Creams that separate or turn grainy. Inhalers that don’t spray properly. If anything looks off, toss it. Don’t wait for the date on the bottle. BeMedWise says 53% of people can’t tell when a medicine has gone bad without a checklist. Mark multi-dose items like insulin vials or eye drops with the date you opened them. Most lose potency after 28 days. Write it right on the bottle with a permanent marker.Dispose of Expired or Unused Meds the Right Way
Flushing meds down the toilet or tossing them in the trash is dangerous-and bad for the environment. The EPA says 60-80% of pharmaceuticals end up in water systems when flushed. The U.S. Geological Survey found traces of drugs in 80% of U.S. streams. Use a drug take-back program. The DEA runs National Prescription Drug Take Back Days twice a year-in April and October. Many pharmacies and police stations also accept old meds year-round. That’s the safest, cleanest way. If no take-back option is nearby, mix pills with something unappetizing: coffee grounds, cat litter, or dirt. Put them in a sealed plastic bag before throwing them in the trash. This cuts accidental ingestion risk by 76%, according to the FDA. Never crush pills before mixing-some are designed to release slowly.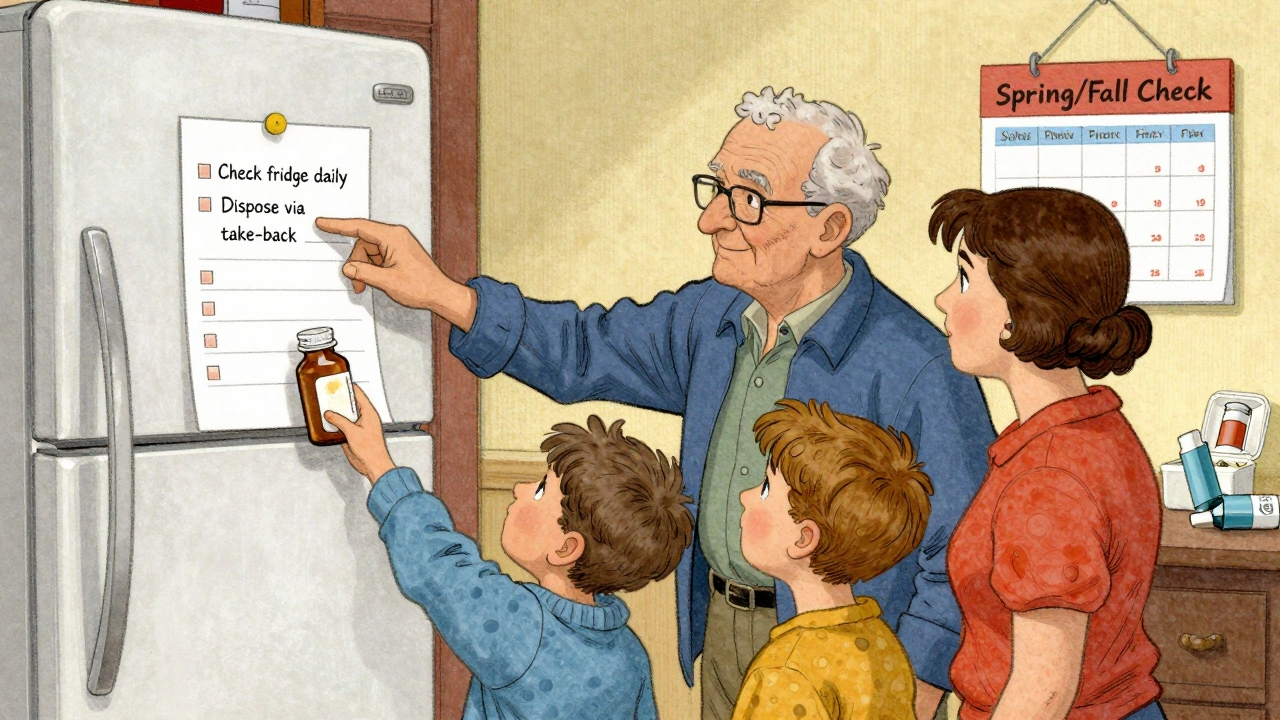
Special Cases: Insulin, Inhalers, and More
Insulin: Keep unopened vials in the fridge. Once opened, store at room temperature. Write the opening date on the vial. Discard after 14-56 days, depending on the type. A 2022 American Diabetes Association study found 38% of users store in-use insulin wrong-cutting its effectiveness by up to 30%. Inhalers: Store them in their original plastic case to prevent accidental activation. Don’t leave them in hot cars or near heaters. Cold temperatures can make them less effective. Keep them in your main storage area, not the bathroom. Topical products: Creams, ointments, and repellents count as medications too. North Carolina’s Kaitlyn’s Law requires all of them to be stored in original containers with labels. This reduces errors by 72%, according to UNC Chapel Hill.Build Your Checklist-Step by Step
Here’s a simple, practical checklist you can print or save on your phone:- ✅ Store all meds in one locked, cool, dry location (not bathroom)
- ✅ Keep meds at least 4 feet off the ground
- ✅ Separate each person’s meds with labeled bins or shelves
- ✅ Mark high-alert meds (insulin, opioids, warfarin) with “High Alert” stickers
- ✅ Refrigerate insulin and other cold-stable meds at 36-46°F
- ✅ Check fridge temp daily-log it
- ✅ Write “opened on” date for multi-dose items
- ✅ Inspect meds every month for color, texture, or smell changes
- ✅ Do full inventory every six months (spring/fall)
- ✅ Discard expired or degraded meds immediately
- ✅ Use drug take-back programs for disposal
- ✅ If no take-back: mix with coffee grounds, seal in bag, trash
Why This Matters More Than You Think
A 2023 Consumer Reports survey of 2,500 households found those using a formal storage checklist had 89% fewer medication-related incidents. That’s not just fewer trips to the ER. It’s fewer hospitalizations. Fewer mistakes. Fewer deaths. This isn’t about being perfect. It’s about being prepared. Medications save lives-but only if they’re stored right. A simple checklist turns chaos into control. It protects kids. It keeps seniors safe. It ensures your insulin still works when you need it most. Start today. Print this checklist. Hang it on the fridge. Or save it on your phone. Set a recurring reminder for next month. You won’t regret it.Can I store all my medications in one place?
Yes-but only if you separate them clearly. Store all medications together in a locked cabinet, but use labeled bins or shelves for each person. Mixing meds increases the risk of accidental ingestion, especially in households with multiple users. Keep high-risk drugs like insulin or opioids in a separate, clearly marked container within the main storage area.
Is it safe to keep medications in the kitchen?
Only if the kitchen is cool and dry. Avoid storing meds near the stove, oven, or dishwasher. Heat and steam can damage pills and liquids. A pantry or cabinet away from cooking areas is fine. But if your kitchen gets hot or humid, pick another spot. A bedroom drawer or linen closet is more stable.
What should I do if I find an expired medication?
Don’t take it. Even if it looks fine, potency may have dropped. Check for discoloration, odd smells, or changes in texture. If in doubt, discard it. Use a drug take-back program if available. If not, mix it with coffee grounds or cat litter, seal it in a plastic bag, and throw it in the trash. Never flush unless the label says to.
Do I need to keep medications in their original bottles?
Yes. Original bottles have the name, dosage, expiration date, and pharmacy info. Removing labels increases the risk of mix-ups, especially for seniors or those with vision issues. Even if you use a pill organizer, keep the original bottle nearby as a backup. North Carolina’s Kaitlyn’s Law requires this for childcare settings-and it’s smart for every home.
How often should I check my medication storage?
Do a full inventory every six months-ideally during daylight saving time changes. Check fridge temperatures daily if you store meds there. Do a quick visual inspection every month: look for changes in color, smell, or texture. Update your checklist each time you refill a prescription or get a new medication.
Are over-the-counter meds and supplements included in the checklist?
Absolutely. Vitamins, pain relievers, antacids, and topical creams all count. They can still be dangerous if taken incorrectly or by the wrong person. Children have been poisoned by chewable vitamins. Seniors have overdosed on OTC sleep aids. Treat every pill the same way-store it safely, label it clearly, and dispose of it properly.


Adam Everitt
December 12, 2025 AT 07:05so i read this and thought wow like why didnt someone tell me this 10 years ago when my kid swallowed my dad’s blood pressure pills
turns out the bathroom cabinet was our ‘med station’ for decades
no joke we thought it was clean cause it had a sink
turns out its basically a steam room for pills
now everything’s in a locked drawer in the hallway
and yeah i even wrapped the insulin in foil cause why not
small changes but feels like i just saved a life
wendy b
December 12, 2025 AT 07:16While the general sentiment of this post is commendable, one must acknowledge the fundamental flaw in its empirical grounding: the FDA’s assertion regarding 50% potency loss in humid environments lacks peer-reviewed citation in the context of ambient household conditions. Furthermore, the recommendation to use aluminum foil for light-sensitive medications is technically correct but ignores the regulatory requirement for original packaging under the U.S. Drug Supply Chain Security Act. One cannot simply repackage controlled substances without violating federal guidelines. This post reads like a well-intentioned blog post masquerading as clinical guidance.
Ashley Skipp
December 13, 2025 AT 02:27you people are so over the top with this checklist nonsense
my grandma kept her meds in a shoebox next to the toaster and lived to 94
if your kid can open a drawer you got bigger problems than pills
and dont even get me started on the ‘high alert’ stickers
its not a military base its your house
Nathan Fatal
December 14, 2025 AT 11:59Wendy’s point about original packaging is valid but misses the bigger picture. The FDA’s guidance on disposal and storage is designed for pharmacies and hospitals, not homes. The real issue is accessibility and human behavior. A locked box with labeled bins doesn’t violate the DSCSA-it protects against accidental ingestion. The 92% reduction in pediatric ingestions from locked boxes is from a peer-reviewed Pediatrics study, not a blog. And yes, foil over clear bottles is a practical workaround for people who don’t have amber containers. The goal isn’t perfection-it’s prevention. If you’re worried about regulatory compliance, use a pharmacy-provided lockbox with original labels intact. But don’t let bureaucracy stop you from doing something that saves lives.
Robert Webb
December 14, 2025 AT 19:39I’ve worked in home healthcare for 18 years and I can tell you this checklist is the most practical thing I’ve seen in a long time. I’ve seen too many seniors mix up their blood thinners with their antidepressants because the bottles looked the same. I’ve seen insulin left on the counter in the summer and it went bad-patients didn’t know until their glucose spiked. I’ve seen teens take their sibling’s ADHD meds because it was just sitting on the nightstand. This isn’t about being paranoid. It’s about creating systems that account for how humans actually live. The six-month inventory during daylight saving? Genius. People already reset their clocks. Use that habit. The locked box? Non-negotiable. Even if you think your kids are ‘good,’ curiosity doesn’t care about your trust. And don’t forget the coffee grounds trick for disposal. It’s messy, yes, but it’s safer than flushing and way more effective than just tossing pills in the trash. This isn’t a chore-it’s a ritual of care. Do it for the people you love. Do it for the version of yourself who doesn’t want to explain to a child why they can’t wake up.
nikki yamashita
December 16, 2025 AT 17:18YES. This. Just printed it and taped it to the fridge. My mom’s insulin was in the bathroom and I didn’t even realize it was a problem. Now it’s in the locked drawer with the labels. Also started writing opening dates on vials. Feels so simple but so powerful. Thank you for this.
Donna Anderson
December 16, 2025 AT 18:42omg i just found 3 expired benadryl in my purse from 2021
and i thought they were fine cause they still looked ok
now im dumping them in coffee grounds and i feel like a better person
also my 8 year old knows the lockbox code now and he’s the one who reminds me to check the fridge temp
weird but kinda sweet
Levi Cooper
December 18, 2025 AT 11:10Why are we letting the government tell us how to store medicine in our own homes? This checklist is just another step toward control. Locked boxes? Surveillance culture. Stickers? You’re turning your family into a pharmacy. In my day, we kept pills in the medicine cabinet and trusted our kids to be careful. America is getting softer by the day. You want safety? Teach your kids responsibility-not lock everything away. This isn’t protection. It’s fear.