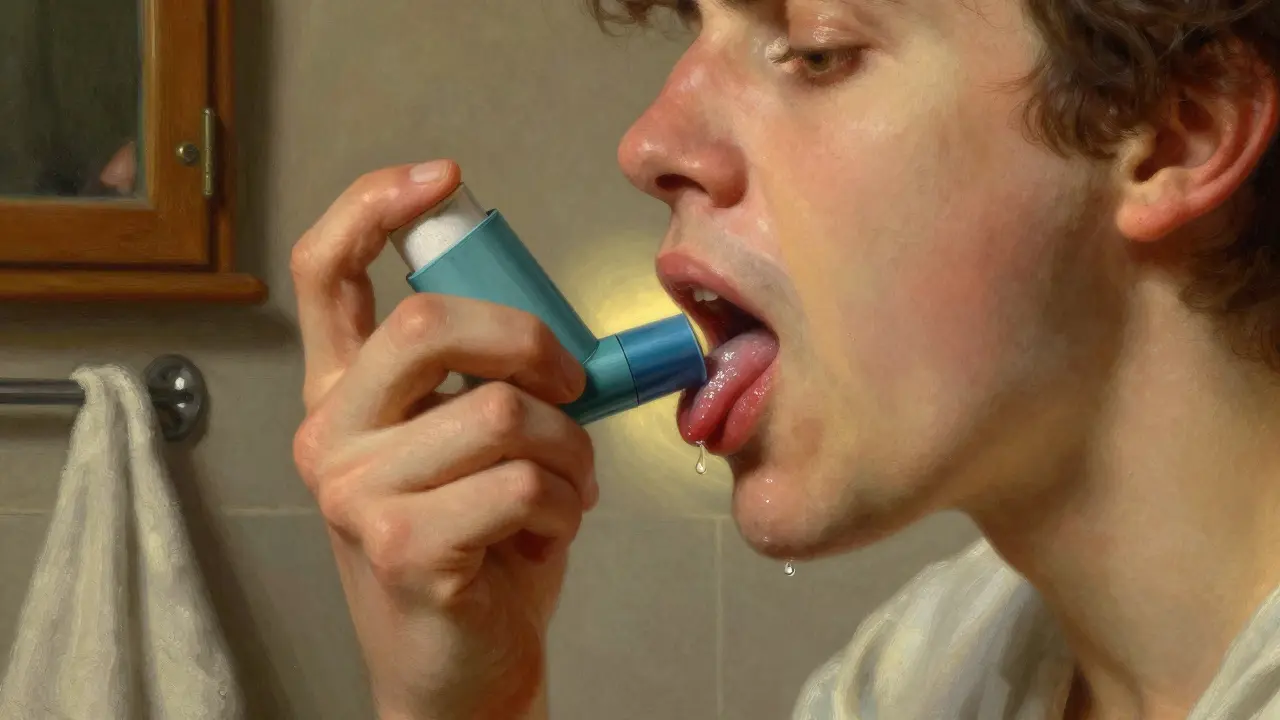
Have you ever opened your mouth in the morning and seen white patches on your tongue or cheeks that won’t brush off? If you’re on long-term asthma inhalers, antibiotics, or immune-suppressing drugs, you’re not alone. Oral thrush is one of the most common but often overlooked side effects of everyday medications. It’s not just uncomfortable-it can make eating, swallowing, and even talking painful. The good news? It’s treatable. And with the right steps, you can stop it from coming back.
Why Medications Cause Oral Thrush
Oral thrush isn’t caused by being dirty or having poor hygiene. It’s caused by an imbalance. Your mouth is full of tiny microbes-bacteria, fungi, viruses-that normally live in harmony. But when certain medications upset that balance, Candida albicans, a type of yeast, takes over. It grows out of control and forms those telltale white, creamy lesions. The biggest culprits? Inhaled corticosteroids for asthma and COPD, broad-spectrum antibiotics, and immunosuppressants after organ transplants or for autoimmune diseases. Inhaled steroids, like those in Advair or Flovent, don’t kill bacteria directly. But they reduce your mouth’s natural defenses. Without enough protective bacteria, Candida spreads. Antibiotics are even more straightforward: they wipe out good bacteria along with the bad ones, leaving Candida with no competition. And if your immune system is suppressed-say, from a transplant or chemotherapy-you simply can’t fight off the overgrowth. The numbers don’t lie. About 5% of healthy people get oral thrush. But for people using inhaled steroids? That jumps to 20%. In the U.S., over 12.9 million people use these inhalers. That’s millions at risk. And for those on immunosuppressants? The risk is even higher.How Antifungal Treatments Work
There are two main ways to treat oral thrush: topical and systemic. Topical means the medicine stays in your mouth. Systemic means it goes into your bloodstream. The choice depends on how bad it is, how strong your immune system is, and what other meds you’re taking. The most common topical treatment is nystatin. It’s been around since the 1950s and still works like a charm. You get a liquid suspension you swish around your mouth for at least two minutes before spitting it out. It doesn’t get absorbed into your body-so it’s safe for kids, pregnant women, and people on multiple drugs. It kills Candida by poking holes in its cell walls. Simple. Direct. Effective. For more serious cases, or if the infection has spread to your throat or esophagus, doctors turn to fluconazole. This is an oral pill. It’s absorbed into your blood and travels to where the infection is. It’s stronger than nystatin and works faster. Studies show it cures 95% of cases within two weeks. It’s the go-to for people with weakened immune systems, like those with HIV or cancer. But here’s the catch: fluconazole can interact with other drugs. It messes with liver enzymes that break down medications like warfarin, phenytoin, and some diabetes pills. It can also cause headaches, stomach upset, and-rarely-liver damage. That’s why doctors don’t jump to it right away. Nystatin is the first line of defense for most people.Comparing Nystatin and Fluconazole
| Feature | Nystatin | Fluconazole |
|---|---|---|
| Form | Oral suspension (liquid) | Oral tablet |
| Dosing | 4 times daily, swish and spit | Once daily |
| Duration | 7-14 days | 7-14 days |
| Effectiveness | 89% for mild cases | 95% for most cases |
| Systemic absorption | Less than 5% | 98% |
| Drug interactions | Minimal | 32+ common medications |
| Cost (generic, 30-day supply) | $15.79 | $23.49 |
| Best for | Mild cases, kids, elderly, pregnant women | Severe cases, immunocompromised, esophageal thrush |
One big reason nystatin gets underused? People don’t use it right. A study found 42% of treatment failures happen because patients swallow the liquid right away. You have to swish. You have to hold it. You have to let it coat your tongue, cheeks, and throat. Spit it out. Don’t rinse. Don’t eat for 30 minutes after. If you don’t, it won’t work.
Fluconazole wins on convenience. One pill a day. No spitting. No mess. But if you’re on blood thinners or have liver issues? It’s not worth the risk. That’s why doctors start with nystatin-and only switch if it doesn’t clear up in 10 days.

How to Prevent Oral Thrush Before It Starts
Treating thrush is easy. Preventing it? That’s where most people slip up. If you use an inhaled steroid, rinse your mouth with water immediately after every puff. Don’t just swish. Don’t gargle. Just rinse and spit. Do it every time. Studies show this cuts your risk by 65%. Some people even use a straw to get the medicine farther back in their throat, away from their tongue and cheeks. Brush your teeth twice a day. Floss daily. Don’t skip dental checkups. Your dentist can spot early signs of thrush before it becomes painful. And if you wear dentures? Clean them every night. Candida loves plastic. If you have diabetes, keep your blood sugar under control. High glucose = food for yeast. Aim for an HbA1c below 7.0%. That’s not just for your heart-it’s for your mouth too. New research shows that probiotics help. Lactobacillus reuteri, a friendly bacteria, can reduce thrush recurrence by 57% when taken alongside antifungals. You can find it in some supplements or even certain yogurts. It’s not a magic fix, but it’s a smart add-on. And here’s something most people don’t know: xylitol helps. It’s a sugar alcohol found in sugar-free gum and mints. It doesn’t feed Candida. In fact, it starves it. A study showed xylitol reduces Candida in the mouth by 40%. Chew a piece after meals. It’s easy. It tastes good. And it works.What to Do When Treatment Fails
Sometimes, even with the right meds, thrush comes back. Why? One reason: resistance. Candida is getting smarter. In 2010, only 3% of strains were resistant to fluconazole. By 2022, that number jumped to 12%. That’s why doctors now test for it in recurrent cases. If thrush keeps coming back, ask for a culture. Don’t just take another pill. Another reason: you didn’t finish the course. People stop when the white patches fade. But the yeast is still hiding. You need to finish the full 7-14 days-even if you feel fine. And sometimes, it’s not thrush at all. Leukoplakia, lichen planus, or even early signs of oral cancer can look like thrush. If it doesn’t clear up after two weeks of treatment, see your doctor again.
What’s New in 2026
The field is evolving. In March 2023, the FDA approved a new form of nystatin: a mucoadhesive tablet called Mycolog-II. It sticks to your mouth lining and releases medicine for up to four hours. No swishing. No spitting. Just place it on your cheek and let it dissolve. Early results show 94% success-better than the liquid. Researchers are also testing new antifungals in clinical trials. Three are in Phase II, designed to be more targeted, with fewer side effects and less chance of resistance. One even works against Candida auris, a dangerous, drug-resistant strain showing up in hospitals. But here’s the bottom line: nystatin isn’t going anywhere. It’s cheap. It’s safe. It works. And with new delivery methods, it’s getting even better.Can oral thrush go away on its own without treatment?
Sometimes, yes-especially if it’s mild and caused by a short course of antibiotics. But if you’re on long-term steroids, immunosuppressants, or have diabetes, it’s unlikely to clear on its own. Waiting can let it spread to your throat or esophagus, making it harder to treat. Don’t risk it. Start treatment early.
Is oral thrush contagious?
Not really. You can’t catch it from kissing or sharing a cup. Candida is already in most people’s mouths. Thrush happens when it overgrows due to medication, poor hygiene, or a weak immune system. It’s an imbalance, not an infection you pass around.
Can I use mouthwash to treat oral thrush?
Regular alcohol-based mouthwashes can make it worse. They kill good bacteria, which lets Candida grow even more. Some antiseptic rinses with chlorhexidine may help temporarily, but they’re not a substitute for antifungal meds. Stick to prescribed treatments and avoid harsh rinses.
Why does nystatin taste so bad?
It’s made from a natural fungus, and the taste is just how it is-chalky, bitter, and unpleasant. That’s why many people stop using it. But the taste doesn’t mean it’s not working. Try chilling the suspension before use-it can dull the flavor. Or mix it with a little applesauce (just don’t swallow it right away). The goal is contact time, not taste.
Can children get oral thrush from medications?
Yes. Babies on antibiotics or inhaled steroids for asthma can get thrush. Nystatin is safe for infants and toddlers. The dose is based on weight, and it’s often applied with a dropper or cotton swab. If your baby has white patches on the tongue that don’t wipe off, see your pediatrician. Don’t assume it’s just milk residue.
How long until I feel better after starting treatment?
Most people notice improvement in 2-3 days. The white patches start to fade, and swallowing gets easier. But don’t stop treatment early. Full healing takes 7-14 days. Stopping too soon is the #1 reason thrush comes back.
Can I drink alcohol while taking fluconazole?
It’s not dangerous, but it’s not smart. Alcohol can worsen fluconazole’s side effects like headaches, nausea, and liver stress. If you’re already feeling off from the medication, adding alcohol just makes it worse. Wait until you’re done with the course.
Should I change my inhaler if I keep getting thrush?
Not necessarily. Switching inhalers won’t fix the problem if you’re not rinsing after use. But if you’re still getting thrush despite rinsing, talk to your doctor. You might need a spacer device to reduce how much medicine lands in your mouth. Or they might switch you to a lower-dose steroid. Prevention is about technique, not just the device.
Final Thoughts
Oral thrush from medications isn’t a sign you’re doing something wrong. It’s a side effect of life-saving treatments. But that doesn’t mean you have to live with it. Nystatin works. Fluconazole works. Prevention works even better. Rinse after your inhaler. Brush your teeth. Chew xylitol gum. Use probiotics. Finish your meds. These aren’t just tips-they’re proven steps that millions use every day to stay healthy.The next time you see white patches in your mouth, don’t ignore them. Don’t wait. Don’t assume it’s just a sore throat. Take action. Your mouth-and your body-will thank you.

Lily Steele
January 30, 2026 AT 08:27Just rinsed my mouth after my inhaler today and thought of this post. Such a simple habit, but it made all the difference. No more white patches. Seriously, if you’re on steroids, do this. It’s free and it works.
Done.
Thanks for the reminder.
Shubham Dixit
February 1, 2026 AT 00:35Look, I’ve been on Advair for 12 years and I’ve seen the whole system break down. The pharmaceutical companies don’t want you to know that nystatin is cheaper than your morning coffee, but they push fluconazole because it’s a cash cow. And don’t get me started on how they silence the research on xylitol because it’s not patentable. This isn’t medicine-it’s a profit-driven circus. You think your dentist cares? They get kickbacks from big pharma for prescribing the expensive stuff. I’ve been using nystatin with a dropper since 2015. My thrush hasn’t returned. No pills. No side effects. Just science. And if you’re not doing it right, you’re not doing it at all. Swish. Spit. Wait. Don’t be lazy. Your mouth isn’t a trash can.
Rohit Kumar
February 2, 2026 AT 02:04There’s a deeper truth here that most miss. The mouth is not just an entryway-it’s a mirror of systemic imbalance. When Candida takes over, it’s not merely a fungal overgrowth. It’s the body screaming that harmony has been shattered. Modern medicine treats symptoms, not roots. We suppress with drugs, never restore with ecology. The real solution isn’t just nystatin or fluconazole-it’s rebuilding the microbial ecosystem. Probiotics, yes. But also fasting, reducing sugar, grounding, breathwork. The body remembers balance. We just forgot how to listen. This isn’t about pills. It’s about returning to rhythm.
Jodi Olson
February 2, 2026 AT 09:51Interesting how the article mentions Candida albicans but doesn’t touch on Candida glabrata or tropicalis which are becoming more common in immunocompromised patients and often less responsive to fluconazole. Also, the cost comparison ignores insurance tiers. In my case, fluconazole was $5 with insurance, nystatin was $47 because it’s not formulary preferred. The data is solid but the real-world access piece is missing. And yes, I’ve had thrush twice since my transplant. Swishing doesn’t always cut it. Sometimes you need the pill. No shame in that.
Carolyn Whitehead
February 3, 2026 AT 15:03I had thrush after antibiotics last year and it was so annoying. I didn’t know about the xylitol thing until now. I’ve been chewing gum after meals ever since and honestly? No more white stuff. Also, I started using a straw with my inhaler and it felt weird at first but now I don’t even think about it. Small changes, big difference. Thanks for sharing this. I’ll pass it along to my mom-she’s on steroids and hates the nystatin taste.
Amy Insalaco
February 4, 2026 AT 03:00Let’s be clear: this article is a beautifully curated piece of pharmaceutical propaganda. The FDA approval of Mycolog-II? A classic example of ‘me-too’ drug innovation-same active ingredient, new delivery mechanism, triple the price. The mucoadhesive tablet is nothing more than a placebo in fancy packaging. Meanwhile, the real innovation-the 57% reduction with Lactobacillus reuteri-is buried under a mountain of fluconazole hype. And let’s not forget the elephant in the room: the microbiome. We’re treating a symptom while ignoring the systemic dysbiosis caused by chronic corticosteroid use, processed diets, and antibiotic overprescription. This isn’t medicine. It’s symptom management disguised as prevention. The real solution? Reduce steroid reliance. But that would require rethinking the entire asthma management paradigm. And nobody wants to do that. Too disruptive. Too expensive. Too inconvenient.
Katie and Nathan Milburn
February 6, 2026 AT 02:40As a clinical pharmacist, I’ve reviewed hundreds of cases of oral thrush in elderly patients on inhaled steroids. The most common failure? Inadequate rinsing technique. Patients are told to rinse, but not how. Many use a sip of water and swallow it. Others rinse for one second. The protocol requires at least 30 seconds of swishing, then spitting. No swallowing. No immediate eating or drinking. We’ve seen success rates jump from 40% to 85% when patients are shown proper technique with a video demonstration. It’s not the drug. It’s the delivery. Education matters. Always.
Marc Bains
February 6, 2026 AT 10:23For anyone who’s ever felt like thrush is your fault-stop. You’re not dirty. You’re not weak. You’re on life-saving meds. That’s the real story here. I’ve seen patients cry because they think the white patches mean they’re failing at health. They’re not. They’re surviving. And the fact that we have nystatin, xylitol, probiotics, and proper rinsing techniques? That’s a win. Don’t let anyone make you feel guilty for needing help. You’re doing the right thing by staying on your meds and learning how to protect yourself. That’s strength.
kate jones
February 6, 2026 AT 13:05Important clarification: while nystatin has minimal systemic absorption, it is not entirely inert in the GI tract. In patients with intestinal permeability or gut dysbiosis, residual nystatin can alter colonic microbiota, potentially contributing to secondary fungal overgrowth. This is rarely documented but appears in case reports among long-term users. Fluconazole, despite its interactions, offers broader tissue penetration and may be preferable in cases of concurrent gastrointestinal Candida colonization. Always consider the whole system-not just the mouth. Also, chlorhexidine mouthwash, while not curative, can be used adjunctively at 0.12% concentration for 14 days to reduce biofilm load prior to antifungal therapy. Not a replacement, but a bridge.
Sheila Garfield
February 7, 2026 AT 04:38My mum had thrush after chemo and we tried everything. The nystatin tasted awful but she stuck with it because she didn’t want to be on pills. We started giving her sugar-free gum with xylitol after every meal and it made such a difference. She said it felt like her mouth was breathing again. Honestly, the simplest things work best. No need to overcomplicate it. Just rinse, chew, and be patient.
Sarah Blevins
February 8, 2026 AT 08:02Let’s address the elephant: the article omits any mention of the rising prevalence of Candida auris in healthcare settings and its cross-resistance to azoles. While fluconazole is effective against C. albicans, it’s useless against C. auris, which is now endemic in many U.S. hospitals. Patients on immunosuppressants are at risk for multidrug-resistant thrush. This piece reads like a marketing brochure for generic nystatin. It ignores emerging resistance patterns, fails to mention echinocandins as salvage therapy, and provides no guidance on when to suspect non-albicans species. This is dangerously incomplete.
Yanaton Whittaker
February 8, 2026 AT 11:40AMERICA NEEDS TO STOP USING THESE INHALERS LIKE THEY’RE CANDY!!! 🇺🇸
They’re flooding our kids with steroids and then acting shocked when they get thrush. It’s not the kid’s fault. It’s the system. Big Pharma is poisoning us for profit. We need a national ban on inhaled steroids for mild asthma. Let’s go back to nebulizers and natural remedies. I’ve been using oregano oil for 3 years. No thrush. No pills. No nonsense. #StopBigPharma
Kathleen Riley
February 9, 2026 AT 06:15The ontological framework of oral thrush reveals a profound epistemological rupture between biomedical reductionism and holistic somatic intelligence. The Candida albicans paradigm, while empirically verifiable, obscures the deeper phenomenological truth: the mouth as a liminal zone between internal and external worlds, where microbial equilibrium reflects existential harmony. To treat with nystatin is to engage in a symbolic act of reterritorialization-a temporary reassertion of order over chaos. But true healing requires a return to pre-industrial rhythms: fermented foods, sunlight, breath, silence. Fluconazole is not a cure. It is a distraction from the real disease: alienation from the body’s innate wisdom.
Beth Cooper
February 10, 2026 AT 05:19Wait-so you’re telling me this whole thing is just about yeast? What if it’s not yeast at all? What if it’s the fluoride in your water? Or the 5G towers? Or the government’s secret microchips in inhalers? I’ve had thrush since 2018. I stopped using my inhaler and switched to organic hemp oil. It’s gone. And my allergies too. The doctors won’t tell you this because they’re paid by the CDC. They don’t want you to know that Candida is just a cover-up for something bigger. I’ve got 17 studies. Want me to send them? You’re not safe. You’re being lied to.