Burning, stinging, and a raw kind of discomfort—these aren’t the symptoms most people talk about when polycystic ovary syndrome (PCOS) comes up. Most hear about missed periods or unexpected hair growth, but when women whisper about vaginal burning, it’s easy for the conversation to hit a nervous pause. The thing is, for a surprisingly large number of women with PCOS, vaginal burning isn’t rare at all. In fact, it’s a hidden trouble no one wants to admit is happening to them. And because hardly anyone is talking about it, finding real answers and relief can leave you feeling pretty lost.
What Connects PCOS and Vaginal Burning? Medical Explanations That Matter
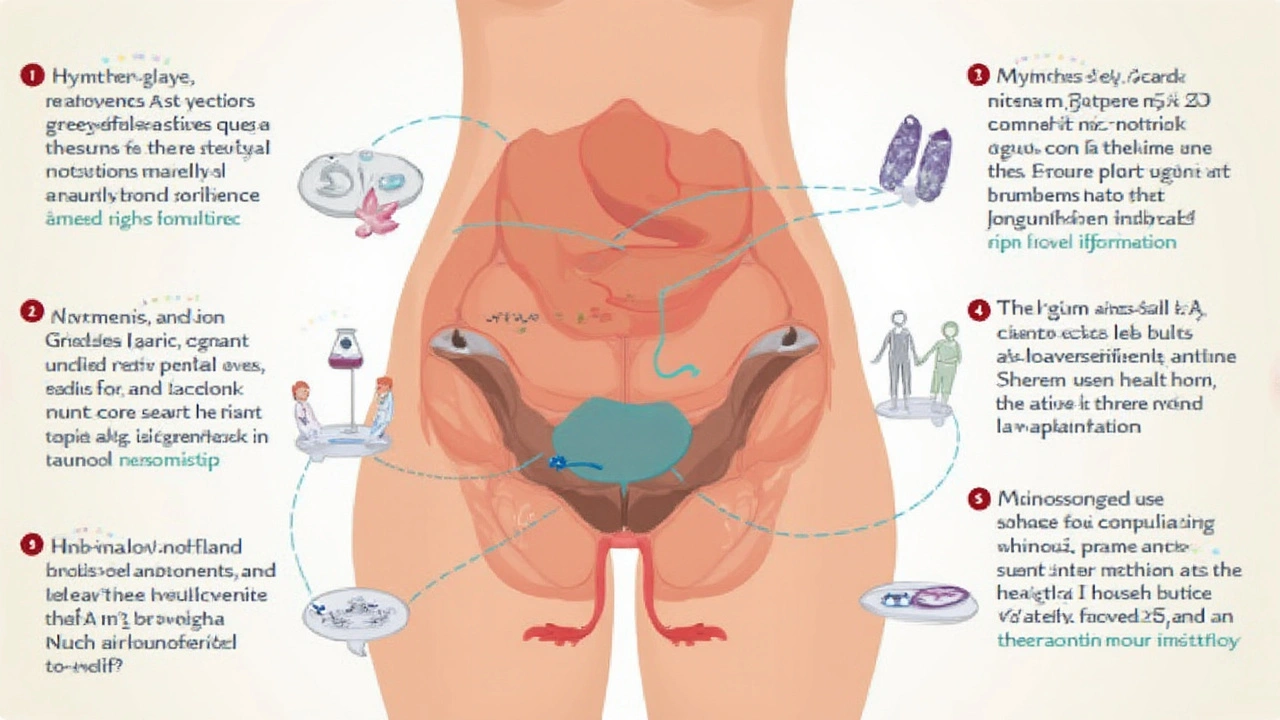
PCOS, or polycystic ovary syndrome, is a complicated condition. At its most basic, it messes with hormones—too much testosterone, not enough estrogen—and that throws lots of body systems out of balance. Classic symptoms like irregular cycles, acne, or extra body hair are easy to Google. Vaginal burning? Not so much, but there are real science-backed reasons why the two go hand in hand.
Here’s where the lightbulb goes on. When your hormones are out of whack, your vaginal tissue can suffer. Estrogen plays a huge role in keeping vaginal tissue healthy, stretchy, and well-lubricated. But PCOS often means low or uneven estrogen, so the tissue gets thinner, fragile, and dry. This dryness isn’t just uncomfortable; it can actually lead to microscopic cracks or sores—opening the door for burning sensations that might flare up all day or get worse during sex, after peeing, or even when sitting for too long.
Another hidden culprit? Blood sugar swings. A lot of women with PCOS deal with insulin resistance, and researchers have found that high blood sugar levels can increase the risk of infections like yeast or bacterial vaginosis. Both love to trigger that raw, burning feeling. Mix in stress—which PCOS tends to dial up even more—and the body’s ability to fight off micro-injuries or infections takes a nosedive. If you toss in tight clothes, scented soaps, or even an enthusiastic session of exercise, the pain and burning can get worse pretty quickly.
Doctors sometimes miss the link between PCOS and vaginal burning because it isn’t yet a “headline” symptom. Most women don’t feel comfortable mentioning it, or their GP rushes to blame it on a simple UTI. But when bloodwork, swabs, and urine tests keep coming back normal, and you still feel that sting, PCOS might be the missing piece of the puzzle. The medical explanation connects the dots: it’s a mix of hormone chaos, dryness, and infection risks from blood sugar roller coasters. Some women figure out the pattern when the burning gets worse before their period or after stressful weeks. Others might notice a burn that comes and goes without rhyme or reason. But the science is there, even if the story isn’t well told yet—until now.

Step-by-Step Strategies: Real Relief for PCOS-Linked Vaginal Burning
Dealing with vaginal burning from PCOS isn’t about finding a miracle fix—it’s about stacking smart changes that help your body heal and adapt. Think of it like repairing a weathered fence: one layer of paint isn’t enough, but a few well-chosen steps can do the trick.
1. Hydration and Gentle Care: Vaginal tissues need moisture to stay healthy. Use a gentle, fragrance-free moisturizer made for the vulva—no body lotions or scented gels here. Coconut oil or a vitamin E balm can help for some people, but always patch test first. Steer clear of bubble baths, douches, and heavily scented pads or liners, which just dry things out more.
- Wipe front to back, and stick to unscented, simple toilet paper.
- Choose loose, breathable underwear (think pure cotton—lace has its place, but not every day).
- If sex makes burning worse, try water-based lubricants—never anything tingling or flavored.
2. Manage Blood Sugar Swings: Insulin resistance isn’t just a PCOS thing; it can set off burning by making you more prone to yeast or bacterial infections. Keep blood sugar steady with balanced meals: lots of veggies, lean protein, and slow-digesting carbs. Avoid bingeing on sweet stuff. Try spacing your meals out so you’re not starving, then feasting and feeling the crash.
- If you take metformin or another medication for PCOS, ask your doctor to check your levels regularly. Some women find that the burning eases up when their blood sugar control improves.
- Probiotics (either in food—like sugar-free yogurt—or as supplements) help the body fend off infection and keep the delicate vaginal balance happy.
3. Soothe and Heal: An oatmeal bath is a time-tested way to calm burning skin, and yes—it helps around the vulva too (just not inside). Anti-inflammatory creams or hydrocortisone (over-the-counter) might be worth a shot, but only for a few days at a time.
One study out of the University of Queensland found that women with PCOS who used vaginal moisturizers two to four times a week reported less burning after four weeks, especially if they added in a probiotic diet. Another small trial even found that topical estrogen creams (when approved by your doctor) offered big improvements—especially for women with severe dryness.
- If burning comes with visible redness or a cottage cheese-like discharge, head to a clinic—yeast or BV needs proper treatment. Don’t try to self-diagnose or use random over-the-counter creams because not every burning is an infection.
- If pain flares after sex, try pausing on intercourse for a week and build up again with extra lubrication (think water-based, paraben-free options).
4. Mental Health, Stress, and Burnout: Stress makes everything worse—especially the body’s ability to heal tissue, reset hormones, and manage pain. If PCOS flares send your anxiety into overdrive, seek backup. Whether that’s a counselor, a PCOS support group, or simply unplugging for an hour, it’s worth it. Women in a Melbourne-based study said mindfulness meditations actually lowered their burning—and it wasn’t a placebo effect; cortisol levels dropped too.
It’s never just “in your head,” but what’s going on inside your head does matter for symptoms like burning. Even getting enough sleep—a rock solid, boring eight hours—can calm inflammation and make the pain easier to cope with.
If you want to dig deeper into the details behind why PCOS triggers burning, check out this clear breakdown on PCOS burning sensation. It lays out the science without drowning you in jargon.
When to Push for Answers and What to Ask Your Doctor
One of the hardest parts of living with PCOS is standing your ground when you know something isn’t right. If burning is a repeating part of your life—and you already know this isn’t just a UTI or yeast issue—it’s time to be blunt about it at the clinic. Some doctors will still brush it off, but spelling out when it started, when it’s worst, and what you’ve already tried makes a difference.
Here’s a handy cheat-sheet to bring to your next appointment if burning is stealing your peace of mind:
- How often does the burning happen—is it constant, then vanishes for days, or comes only after sex, exercise, or peeing?
- Any changes with discharge—color, smell, thickness?
- Are you on birth control, metformin, or any new medications?
- Did the burning start after a change in laundry soap, lubes, underwear, or sex partners?
- Anything make it better or worse, like baths, lotions, or what you eat?
Ask your doctor straight up if you might have low estrogen (sometimes a blood test or trial run with a patch or cream can help). If there’s a whiff of yeast or BV, request both swabs and a pH test—not just a one-minute glance. If insulin resistance hasn’t been checked, now’s the time. And if your doctor seems lost, ask for a referral to a women’s health specialist or endocrinologist familiar with PCOS. In some cities, there are sexual health clinics with expert teams ready for exactly this.
Finally—don’t let shame or frustration steal your sleep. Vaginal burning happens to thousands of women with PCOS, but real relief is possible. A mix of hormone tweaks, smart self-care, blood sugar control, and a little patience can calm the flames. You’re not the only one out there googling in the quiet hours, and there’s more help around the corner than you think. Even if it takes a few tries to get there—don’t quit.


Justyne Walsh
May 24, 2025 AT 21:10Oh great, another miracle cure for PCOS that apparently involves sprinkling fairy dust on your genital area. As if we needed another "expert" telling us to ditch all scented products and start rubbing coconut oil like it’s a spa day for the vagina. Sure, because the real cause of hormonal chaos is definitely the brand of underwear you wear, not the complex endocrine dysregulation that takes years of research to untangle. And let’s not forget the ever‑present, totally unbiased suggestion to “just drink more water” while the rest of us are battling insulin resistance that would make a sugar‑loving raccoon jealous. 🙄
Callum Smyth
May 24, 2025 AT 22:53Hey everyone, I totally get how overwhelming this can feel, but you’re not alone in this journey 😊. Small, consistent steps like swapping to fragrance‑free wipes and keeping an eye on blood‑sugar spikes can really make a difference over time. Remember to be gentle with yourself-stress relief techniques like short walks or breathing exercises can help lower cortisol, which in turn may ease the burning. If you notice an infection, don’t wait; proper treatment can break the cycle fast. Keep tracking what works and what doesn’t; you’ll eventually find a routine that eases the discomfort.
Xing yu Tao
May 25, 2025 AT 21:06In contemplating the intricate interplay between polycystic ovary syndrome and the manifestation of vulvar discomfort, it becomes evident that the pathophysiology extends beyond mere superficial observations. The dysregulation of the hypothalamic‑pituitary‑ovarian axis precipitates an elevation in androgenic activity, which concomitantly suppresses aromatase conversion, thereby diminishing estradiol availability for mucosal maintenance. This estrogenic insufficiency compromises the integrity of the vaginal epithelium, rendering it susceptible to micro‑abrasions and subsequent nociceptive signaling. Moreover, insulin resistance, a hallmark of PCOS, introduces hyperglycemic excursions that foster an environment conducive to opportunistic microbial proliferation, notably Candida albicans and bacterial vaginosis agents.
From a therapeutic standpoint, a multimodal approach is requisite. Firstly, the judicious administration of topical estrogenic preparations can restore epithelial thickness, yet this must be balanced against oncogenic risk profiles. Secondly, systemic insulin‑sensitizing agents, such as metformin, have demonstrated efficacy in attenuating glycemic volatility, thereby indirectly mitigating inflammation. Thirdly, the incorporation of probiotic lactobacilli may reestablish vaginal flora equilibrium, reducing pathogenic colonization.
Psychosocial considerations are equally paramount. Chronic pain conditions, including persistent vulvar burning, exert a deleterious impact on mental health, potentially exacerbating hypothalamic stress responses that further perturb hormonal homeostasis. Hence, integrative interventions encompassing mindfulness‑based stress reduction, cognitive behavioral therapy, and supportive peer networks should be advocated alongside biomedical modalities.
In summation, the confluence of hormonal insufficiency, metabolic instability, and microbial dysbiosis delineates a complex etiological tapestry. Addressing each constituent with evidence‑based strategies-topical estrogen, insulin sensitizers, probiotic supplementation, and psychosocial support-offers the most comprehensive avenue toward amelioration of PCOS‑related vaginal burning.
Adam Stewart
May 25, 2025 AT 22:30A thoughtful perspective, thank you.
Selena Justin
May 27, 2025 AT 00:53I appreciate the compassionate tone of the previous comments and would like to add that staying hydrated internally can also influence mucosal health. Drinking adequate water supports overall tissue elasticity and may reduce the sensation of dryness. Additionally, incorporating omega‑3 rich foods such as flaxseed or walnuts can help modulate inflammatory pathways, which sometimes exacerbate burning sensations. Remember, you deserve patience and kindness from yourself as you experiment with these adjustments.
Bernard Lingcod
May 28, 2025 AT 04:40It’s fascinating how a seemingly localized symptom can actually be a window into systemic metabolic balance; even subtle shifts in glycated hemoglobin can tip the scales toward yeast overgrowth. While the article outlines several practical steps, a less discussed avenue is the role of vitamin D status-deficiency has been linked to increased susceptibility to vaginal infections. Regular, safe sunlight exposure or supplementation might therefore serve as an adjunctive measure in managing PCOS‑related irritation.