H2 Blockers: What They Are, How They Work, and What You Need to Know
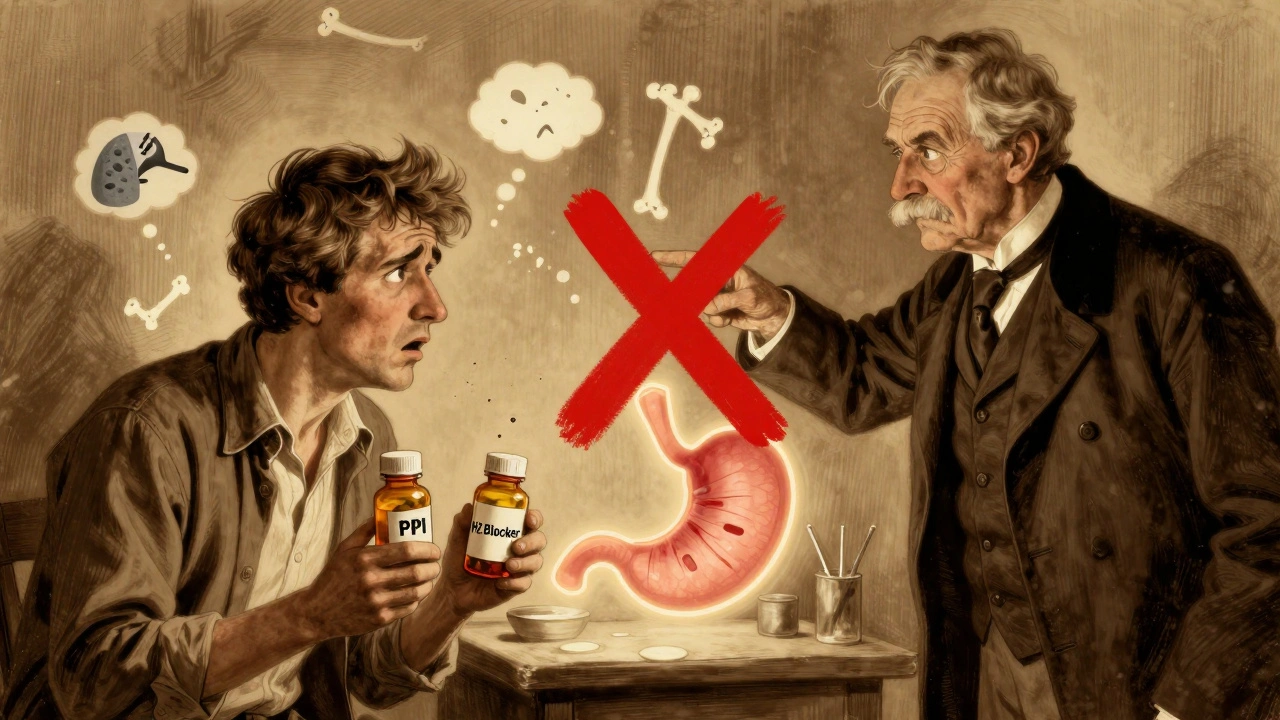
When your stomach makes too much acid, it can cause heartburn, ulcers, or gastritis. That’s where H2 blockers, a class of medications that reduce stomach acid by blocking histamine receptors in the stomach lining. Also known as histamine H2-receptor antagonists, they’re one of the most common ways to calm down acid-related discomfort without reaching for stronger drugs. Unlike proton pump inhibitors (PPIs), which shut down acid production at the source, H2 blockers act like a volume knob—turning down acid output, not cutting it off completely.
They’re used for more than just occasional heartburn. People with peptic ulcers, open sores in the stomach or small intestine often caused by H. pylori bacteria or long-term NSAID use use them to let the lining heal. Those with gastritis, inflammation of the stomach lining from stress, alcohol, or infection find relief from the burning sensation. Even people with acid reflux who don’t want daily PPIs turn to H2 blockers for nighttime control or after meals.
Common H2 blockers include famotidine (Pepcid), ranitidine (though mostly pulled from the market), cimetidine (Tagamet), and nizatidine (Axid). They work fast—often within an hour—and last 6 to 12 hours. That’s why many take them before bed to prevent nighttime acid surges. They’re available over the counter, but doctors still prescribe them for longer-term use, especially when combined with antibiotics for ulcers.
They’re not perfect. Some people get headaches, dizziness, or diarrhea. Cimetidine can interfere with other meds because it affects liver enzymes—something you’ll want to talk about if you’re on blood thinners, antidepressants, or seizure drugs. But for most, they’re a safe, predictable way to manage acid without the long-term risks tied to PPIs.
What you’ll find in the posts below isn’t just a list of H2 blocker articles. It’s a collection of real-world insights: how other conditions like kidney disease or heart failure change how your body handles these drugs, why some people still get symptoms even when taking them, and how drug interactions—like with antibiotics or supplements—can make them less effective or even risky. You’ll see how dosage, timing, and individual health profiles make a difference. This isn’t theory. It’s what people actually deal with when they’re trying to feel better without making things worse.