Type A and B Reactions: What They Are and How They Affect Your Medications
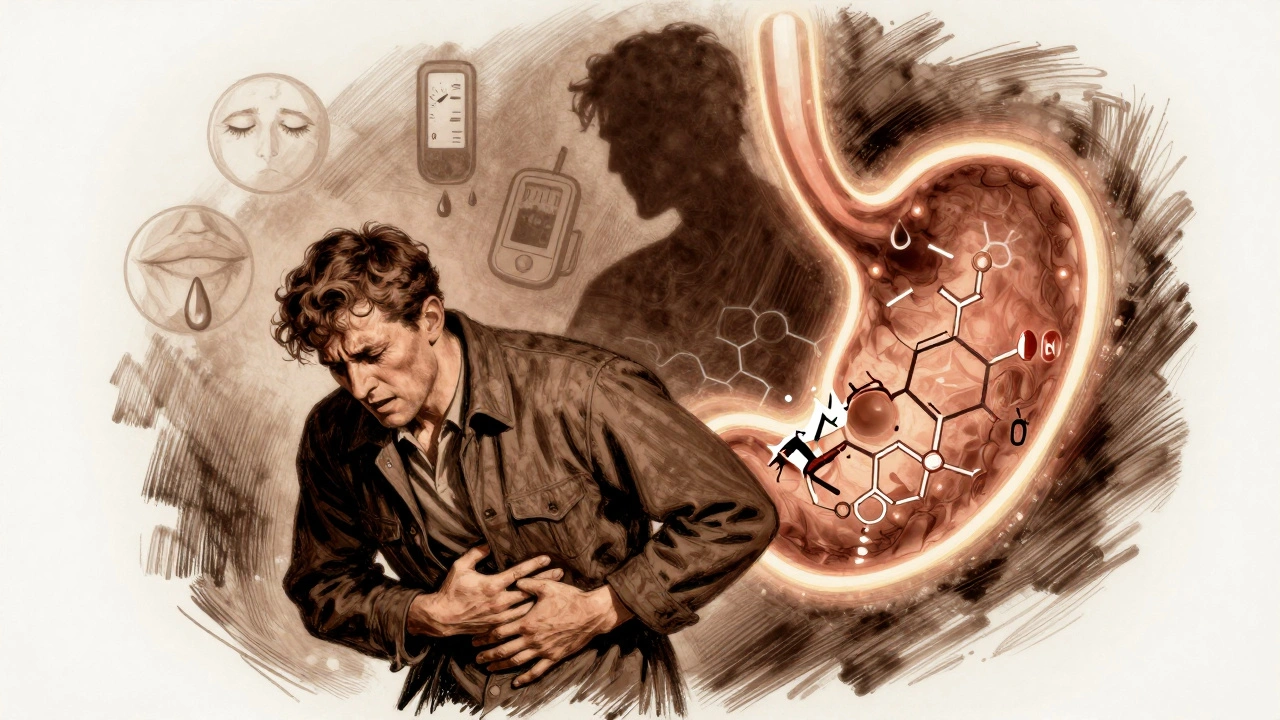
When a medication causes an unwanted effect, it’s not always the same kind of problem. Type A reactions, predictable side effects tied to a drug’s known pharmacology. Also known as augmented reactions, they happen because the drug does too much of what it’s supposed to do—like drowsiness from sleep aids or low blood pressure from blood pressure meds. These are the most common, often dose-dependent, and usually show up in clinical trials. On the flip side, Type B reactions, unpredictable, immune-driven responses that aren’t linked to the drug’s main action. Also known as bizarre reactions, they’re rarer but can be life-threatening—like anaphylaxis from antibiotics or severe skin rashes from anticonvulsants. Think of Type A as the expected cost of taking a drug. Type B? That’s your body saying, "I don’t recognize this."
Most people know about side effects, but few realize how differently these two types behave. Type A reactions show up in drug labels, are often preventable by adjusting the dose, and affect people with certain health conditions—like how kidney disease turns common painkillers into risks. That’s why comorbidities and drug interactions show up so often in our posts. Immunogenicity, how your immune system reacts to biologics or biosimilars, is a classic Type B trigger. It doesn’t matter if you’ve taken the drug before—this time, your body might suddenly see it as an invader. That’s why some patients on tacrolimus develop tremors even when blood levels are normal, or why someone might react badly to a biosimilar that’s "identical" to the original. Meanwhile, drug interactions, when two meds change each other’s effects in the body—like tizanidine and ciprofloxacin causing dangerous drowsiness—are usually Type A. They’re avoidable with better awareness.
Understanding the difference saves lives. Type A reactions are managed by stopping the drug, lowering the dose, or switching to something safer—like choosing a hydrophilic statin to cut muscle pain risk. Type B reactions? You stop the drug, never use it again, and carry an epinephrine pen if you’re at risk for anaphylaxis. These aren’t just medical terms—they’re practical filters for deciding what to watch for. Our collection dives into real cases: how OTC sleep aids cause memory issues (Type A), why combining acid meds increases infection risk (Type A), and how a single antibiotic can trigger a rare immune response (Type B). You’ll find guides on spotting hidden dangers in supplements, reading labels for interactions, and knowing when a side effect is just annoying versus truly dangerous. This isn’t theory. It’s what happens when your body meets your medicine—and what you need to do next.