Why Vaccines Don’t Always Work the Same Way in People on Immunosuppressants
When you’re on medication that shuts down part of your immune system-whether for rheumatoid arthritis, lupus, Crohn’s disease, or after a transplant-getting vaccinated isn’t as simple as showing up for a shot. The vaccines still matter, maybe even more. But they often don’t work as well. Studies show people on these drugs can have 30% to 80% lower antibody responses compared to healthy adults. That doesn’t mean skip the shot. It means you need to time it right.
Best Time to Get Vaccinated: Before You Start Treatment
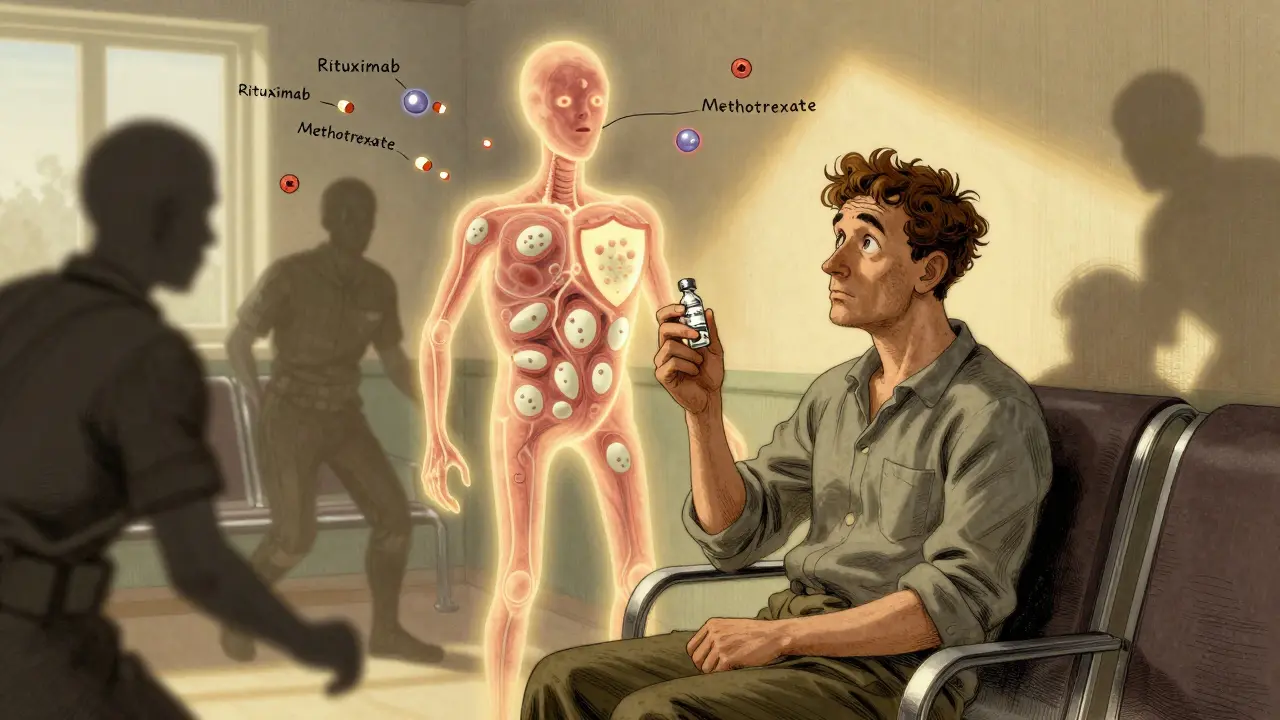
If you know you’re going to start immunosuppressive therapy-like rituximab, methotrexate, or high-dose prednisone-the best window is at least two weeks before your first dose. This isn’t just a suggestion. It’s backed by CDC and IDSA guidelines. Why? Because your immune system still has its full strength before the drugs start dampening it. Vaccines need active immune cells to build a good response. Once those cells are suppressed, the vaccine can’t do its job properly.
For example, if you’re scheduled to begin rituximab for rheumatoid arthritis, getting your flu shot or COVID-19 vaccine two weeks before your infusion gives your body a fighting chance. Waiting until after you’ve started treatment? That’s like trying to build a house after the foundation has been washed away.
Timing Vaccines Around Specific Drugs
Not all immunosuppressants work the same way, so timing matters differently for each.
- Rituximab and other B-cell depleters (like obinutuzumab): These drugs wipe out the immune cells that make antibodies. If you get vaccinated while they’re still active, your body can’t respond. Experts recommend waiting 4 to 6 months after your last infusion before getting any vaccine. Some transplant centers even suggest waiting 9 to 12 months for the best results. But if community COVID-19 cases are spiking, don’t wait. Get the vaccine anyway. The risk of infection outweighs the risk of a weaker response.
- Methotrexate: If you’re on this for psoriasis or arthritis, hold your flu shot for two weeks after vaccination. This small pause lets your immune system focus on building protection instead of fighting the drug. Your rheumatologist can help you adjust your schedule without risking a flare.
- Prednisone at 20mg or higher daily: High doses suppress immune responses broadly. If possible, delay non-flu vaccines until you’re down to under 20mg a day. For flu shots, it’s okay to proceed-just know the protection might be weaker.
- Chemotherapy: Timing depends on your cycle. For drugs like cyclophosphamide or obinutuzumab, aim to vaccinate in the week before your next infusion. That’s when your white blood cell count is usually highest. Talk to your oncologist. They track your counts and can pick the best day.
What About After a Transplant?
People who’ve had a kidney, liver, or heart transplant are especially vulnerable. The immune system is kept low on purpose to prevent rejection. So when should you get vaccinated?
Most guidelines agree: wait at least three months after transplant. Some say one month is okay, but three months gives your body a better shot. Don’t get vaccinated during active rejection episodes or while you’re getting high-dose steroids to treat rejection. That’s when your immune system is being pushed even further down. Wait until things stabilize.
Also, don’t forget the basics. Get your pneumococcal, hepatitis B, and Tdap shots if you haven’t already. These aren’t optional. They’re lifesavers for transplant patients.
Why Some Vaccines Are Safer Than Others
Live vaccines-like MMR, varicella, and nasal flu spray-are off-limits for most immunosuppressed people. Why? Because even weakened live viruses can cause serious infections if your immune system can’t control them.
Stick to inactivated or mRNA vaccines: flu shots (injectable), COVID-19 mRNA vaccines (Pfizer, Moderna), pneumococcal, tetanus, and hepatitis B. These don’t contain live viruses. They’re safe. And they’re your best defense.
Even though they’re safer, they still don’t work as well. That’s why extra doses matter. The CDC now recommends that immunocompromised adults get at least one dose of the current season’s COVID-19 vaccine-and often more, depending on your history. Some patients need three or four doses just to get a decent response.
Real-World Effectiveness: What the Numbers Really Show
Numbers can be misleading. One study found mRNA vaccines were 94% effective in healthy people against COVID-19. In people with autoimmune diseases on immunosuppressants? It dropped to 80.4%. That’s still good-but not great. Another study showed solid organ transplant patients had 56% lower antibody levels after two mRNA doses compared to healthy controls.
Here’s the twist: antibodies aren’t the whole story. Your T-cells might still be working, even if your antibody levels are low. That’s why you still get some protection. It’s not perfect, but it’s better than nothing. That’s why doctors still push for vaccination-even if you’re on rituximab or high-dose steroids.
The Big Problem: No Test to Measure Your Immune Readiness
Here’s the frustrating part: there’s no blood test your doctor can run to say, “Your immune system is ready now.” We’re stuck using fixed time windows-6 months after rituximab, 3 months after transplant-because we don’t have better tools.
But that’s changing. The NIH just launched a $12.5 million study to see if measuring CD19+ B-cell counts can tell us when it’s safe to vaccinate. If this works, we’ll move from guessing to precision timing. Until then, we’re doing the best we can with what we have.
What Happens If You Miss the Window?
You didn’t get your flu shot before starting methotrexate? You’re already three months into rituximab and just realized you forgot your pneumonia shot? Don’t panic. Get the vaccine anyway.
Yes, the response might be weaker. But if you’re in a high-risk group-older, diabetic, living with someone who’s immunocompromised, or in a community with high infection rates-getting the shot now is still better than waiting for the “perfect” time. That perfect time might never come.
Some experts say: “It’s better to be vaccinated late than never.” Especially with COVID-19, flu, and RSV circulating, the risk of getting sick far outweighs the risk of a less-than-perfect vaccine response.
How to Make This Work in Real Life
Getting the right vaccine at the right time isn’t just your job. It’s a team effort.
- Keep a list of all your medications and when you take them.
- Set a reminder 6 weeks before your next infusion or treatment cycle.
- Ask your rheumatologist, oncologist, or transplant team: “When’s the best time to get my next vaccine?”
- Don’t assume your primary care doctor knows your full treatment plan. Share your medication list.
- Track your vaccine history. If you’ve had multiple doses of the COVID-19 vaccine, make sure your doctor knows.
One study found nearly half of transplant centers didn’t follow timing guidelines because of poor communication between specialists and primary care. Don’t let that be you. Be your own advocate.
What’s Next? Better Tools Are Coming
Scientists are working on ways to measure immune response in real time-not just counting B-cells, but testing how well your body responds to a vaccine challenge. Imagine a simple blood test after your shot that tells you if you’re protected. That’s the goal.
In the meantime, follow the current guidelines. Get vaccinated. Get extra doses if recommended. Hold methotrexate for two weeks. Time your shots around your infusions. And remember: even a weak immune response is better than none at all.
Final Thought: Vaccines Are Still Your Best Shield
Being immunosuppressed doesn’t mean you’re defenseless. It means you need to be smarter about how you use your tools. Vaccines aren’t perfect for you-but they’re still the most powerful thing we have to keep you out of the hospital. Don’t skip them. Don’t delay them unless you have a clear, medical reason. And when in doubt? Get the shot. Your future self will thank you.

Jhoantan Moreira
February 3, 2026 AT 11:36Mandy Vodak-Marotta
February 4, 2026 AT 00:50pradnya paramita
February 4, 2026 AT 06:20Keith Harris
February 5, 2026 AT 20:36Caleb Sutton
February 6, 2026 AT 18:32caroline hernandez
February 6, 2026 AT 21:25Prajwal Manjunath Shanthappa
February 7, 2026 AT 05:08Shelby Price
February 8, 2026 AT 16:51Samuel Bradway
February 9, 2026 AT 06:59Daz Leonheart
February 11, 2026 AT 03:15Alex LaVey
February 11, 2026 AT 04:07Joy Johnston
February 12, 2026 AT 10:59Jamillah Rodriguez
February 13, 2026 AT 21:35Alec Stewart Stewart
February 14, 2026 AT 19:14