Stopping benzodiazepines cold turkey can be dangerous. If you’ve been taking them for more than a month-especially daily-sudden discontinuation can trigger seizures, extreme anxiety, hallucinations, or even life-threatening complications. Yet, millions of people are stuck on these medications long after they were meant to be used. The good news? You don’t have to stay on them. With the right plan, tapering off benzodiazepines safely is not only possible-it’s common.
Why Tapering Matters More Than Ever
Benzodiazepines like alprazolam (Xanax), lorazepam (Ativan), and clonazepam (Klonopin) were designed for short-term relief of anxiety or insomnia. But in the U.S. alone, over 30 million adults used them in 2022, and nearly 1 in 6 used them for more than four months. That’s a lot of people relying on drugs that carry real risks: memory problems, increased fall risk in older adults, cognitive decline, and dependence that builds quietly over time. The 2024 Joint Clinical Practice Guideline, backed by 10 major medical societies, now says clearly: if the risks of long-term use outweigh the benefits, tapering should be the next step. This isn’t just advice-it’s becoming standard care. The FDA required label changes in 2019 warning against abrupt stops. States like California and New York now mandate tapering plans for prescriptions over 90 days. Veterans Affairs cut long-term benzo use by 24% between 2020 and 2023 by making tapering mandatory for high-risk patients.How Fast Should You Taper?
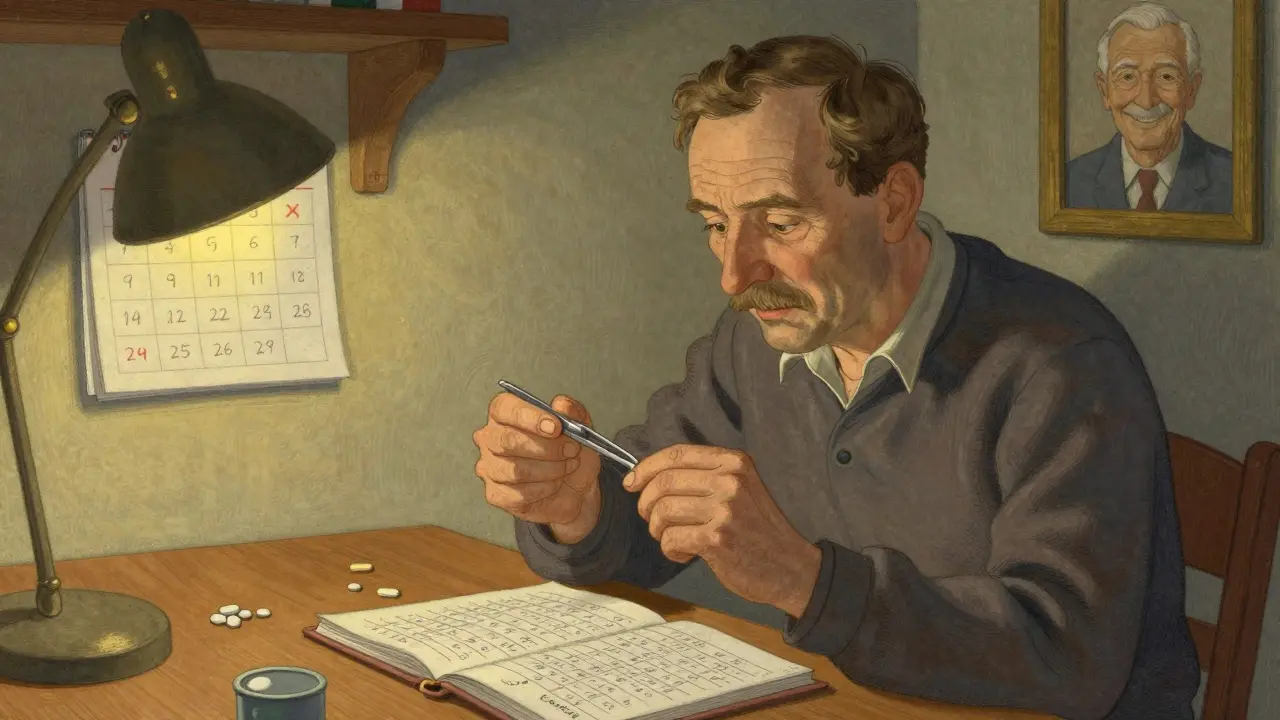
There’s no universal speed. Tapering too fast increases withdrawal risk. Too slow can make you obsessed with the process, worsening anxiety. The key is balance. Most experts agree on starting with a 5% to 10% reduction every 2 to 4 weeks. For someone on 10 mg of diazepam daily, that means cutting 0.5 to 1 mg every few weeks. If you’ve been on benzos for less than 8 weeks, a 2-week taper may be enough. For 6 months to a year, aim for at least 8 weeks. If you’ve been taking them for over a year, 6 to 18 months is typical. Here’s a simple breakdown:- 2-8 weeks of use: 2-week taper
- 8 weeks-6 months: 4-8 week taper
- 6 months-1 year: 8-12 week taper
- Over 1 year: 6-18 month taper
The Three Main Tapering Approaches
There are three proven ways to taper, and your doctor will help you pick the best one based on your history.- Stay on the same drug - Reduce your current benzo by small, regular cuts. Works best for long-acting ones like clonazepam or diazepam.
- Switch to diazepam - This is the gold standard for most people, especially if you’re on short-acting benzos. It’s easier to measure small reductions and your body adjusts more smoothly.
- Add supportive meds - Sometimes, doctors use medications like fluoxetine (Prozac) or certain anticonvulsants to ease withdrawal symptoms. This isn’t a replacement for tapering-it’s a tool to make it tolerable.
What Withdrawal Symptoms to Expect
Withdrawal isn’t the same for everyone. Some people feel nothing. Others have a rough few weeks. Symptoms usually appear 1-4 days after a dose reduction and peak within a week. Common signs include:- Increased anxiety or panic attacks
- Insomnia or vivid nightmares
- Tremors, muscle twitches, or stiffness
- Sensory sensitivity (lights, sounds feel too loud)
- Heart palpitations or dizziness
- Nausea, sweating, or headaches
Who Should Prioritize Tapering?
Not everyone needs to quit. But these groups are at higher risk and should strongly consider tapering:- Adults over 65 - Benzodiazepines double the risk of falls and hip fractures in older adults. The Beers Criteria lists them as potentially inappropriate for seniors.
- People with PTSD or chronic pain - Studies show benzos reduce the effectiveness of trauma therapies and increase death risk in this group.
- Those with a history of substance use - Benzos can trigger relapse or worsen addiction patterns.
- Anyone on multiple sedatives - Mixing benzos with opioids or alcohol is extremely dangerous.
- People taking them for more than 3 months without a clear plan to stop.
How to Make Tapering Work
Tapering isn’t just about pills. It’s about rebuilding your nervous system. Here’s what actually helps:- One prescriber, one pharmacy - Prevents accidental double-dosing or diversion. Keeps your plan clean.
- Weekly check-ins - Your doctor needs to see you regularly to adjust the taper based on symptoms. Don’t wait until you’re in crisis.
- Time-limited refills - Get prescriptions for 1-2 weeks at a time. This forces structure and prevents stockpiling.
- Therapy is non-negotiable - Cognitive Behavioral Therapy (CBT) for anxiety or insomnia is the most effective long-term solution. Studies show 68% success with CBT + tapering vs. 42% with tapering alone.
- Peer support - Talking to someone who’s been through it reduces isolation. VA programs use peer mentors with lived experience-and they work.
What If Symptoms Get Too Bad?
It’s okay to slow down. If you’re having severe symptoms, pause the taper for 1-2 weeks. Stay at your current dose until things stabilize. Then try another 5% cut. Never go back to your old dose to “feel normal.” That resets your progress and makes the next taper harder. Instead, talk to your doctor about temporary, low-dose support meds like melatonin for sleep or beta-blockers for heart palpitations.The Future of Tapering
New tools are emerging. The NIH is funding a mobile app that tracks withdrawal symptoms in real time and suggests dose adjustments based on your input. It’s still in testing, but early results are promising. Health systems are moving toward team-based care: pharmacists managing doses, therapists handling anxiety, peer coaches offering support. This model is already reducing relapse rates in VA clinics. In the next 3-5 years, tapering will become routine-not a last resort. But right now, you have to be your own advocate. Ask your doctor: “Is this still the right medication for me?” “What’s my plan to reduce it?” “Can we add therapy?”When Tapering Isn’t the Right Choice
Some people truly benefit from low-dose, long-term benzos. If you have treatment-resistant anxiety, severe PTSD, or epilepsy-and every other option has failed-staying on a minimal dose might be safer than risking withdrawal. But even then, you should review your need every 3-6 months. The goal isn’t to never use them. It’s to never use them longer than necessary.Can I taper off benzodiazepines on my own?
It’s not recommended. Even though some people try to taper alone, the risk of seizures, severe anxiety, or relapse is much higher without medical supervision. Withdrawal symptoms can escalate quickly, and having a doctor monitor your progress, adjust your plan, and provide support makes a huge difference in safety and success.
How long does benzodiazepine withdrawal last?
Acute withdrawal usually lasts 2-8 weeks after the last dose, depending on the drug and your taper speed. Some people experience protracted symptoms-like sleep issues or mild anxiety-for months, but these are usually less intense and improve with time and support. Most people feel significantly better by 6 months after finishing their taper.
Is diazepam (Valium) really better than other benzos for tapering?
Yes, for most people. Diazepam has a long half-life, meaning it stays in your system longer and releases slowly. This smooths out the peaks and valleys of withdrawal. Switching from a short-acting benzo like Xanax to diazepam is a standard clinical practice because it reduces symptom severity and makes dose reductions easier to manage.
Can I use marijuana or alcohol to help with withdrawal symptoms?
No. Alcohol is a CNS depressant and can interact dangerously with benzodiazepines, increasing overdose risk. Marijuana may temporarily ease anxiety but can worsen sleep and trigger panic in some people. Neither addresses the root issue and can delay real recovery. Stick to proven, non-addictive strategies like therapy, sleep hygiene, and mindfulness.
What if I relapse and go back to my old dose?
Relapse doesn’t mean failure. It means your taper plan needs adjustment. Going back to your old dose resets your tolerance and makes the next taper harder. Talk to your doctor immediately. You may need to slow down, add therapy, or try a different approach. Many people need multiple attempts before they succeed. What matters is you keep trying.

Sidra Khan
December 22, 2025 AT 15:38Wow, finally someone wrote this without sounding like a pharmaceutical ad. I tapered off Xanax after 3 years and it was hell-but the worst part was how no doctor ever warned me it’d feel like my brain was rewiring itself in real time. Now I sleep better than I did on pills. 🌱
Jeffrey Frye
December 22, 2025 AT 16:56lol u think this is science? the fda changed labels bc lawsuits, not because benzos are 'dangerous'. i've been on klonopin 12 years and i'm fine. my brain works better than yours. stop fearmongering.
Aurora Daisy
December 23, 2025 AT 01:24Oh great, another American medical dictatorship post. In the UK, we just prescribe and move on. If you can’t handle withdrawal, maybe you shouldn’t have started. Also, therapy? Please. I’ll take my 2mg diazepam and my tea, thank you very much.
Lu Jelonek
December 23, 2025 AT 16:06For anyone reading this: if you’re considering tapering, find a doctor who’s done this before. Not just any GP. Look for addiction specialists or psychopharmacologists. I was on 8mg of lorazepam for 5 years. Switched to diazepam, cut 0.5mg every 3 weeks. Took 11 months. No seizures. No psychosis. Just quiet, steady healing. You can do this.
Andrea Di Candia
December 25, 2025 AT 00:19It’s funny how we treat chemical dependence like a moral failure instead of a neurological adaptation. The body doesn’t care about your willpower-it just wants balance. Tapering isn’t about quitting. It’s about coming home to yourself. Slowly. Gently. Without shame.
Wilton Holliday
December 26, 2025 AT 16:28Just wanted to say thank you for this. My sister just finished her 14-month taper and she’s laughing again. Not the fake kind-the real one. If you’re reading this and scared? You’re not alone. I’ve been in your shoes. You’ve got this. 💪
bharath vinay
December 27, 2025 AT 13:18They're lying. The whole tapering thing is a psyop to make you dependent on therapists and 'support groups'. Benzodiazepines are natural brain regulators. The real danger is the FDA, Big Pharma, and your doctor pushing you to 'heal' so they can sell you CBT subscriptions. Wake up.
suhani mathur
December 28, 2025 AT 10:00My uncle in Delhi was on clonazepam for 18 years. Switched to diazepam. Cut 1mg every month. Took 2 years. Now he hikes every Sunday. No meds. No panic. Just chai and birds. India’s got this figured out-no fancy apps needed.
Harsh Khandelwal
December 29, 2025 AT 14:04they told me to taper but my doc was a clown who gave me a spreadsheet and said 'good luck'. meanwhile i was shaking so bad i dropped my phone in the toilet. 3 months later i went back to my old dose. i'm not a failure. the system is.
Ademola Madehin
December 31, 2025 AT 11:40bro i tried to taper and my anxiety hit like a truck. i screamed at my cat for 45 minutes. she left. i cried. i called my ex. she didn’t answer. now i’m back on 2mg. i don’t care what the guidelines say. my peace is worth more than your ‘science’.
Pankaj Chaudhary IPS
January 1, 2026 AT 01:12As a medical professional in India, I’ve seen firsthand how stigma prevents patients from seeking help. Tapering isn’t weakness-it’s courage. Many of my patients fear judgment from family or employers. We need community education, not just clinical protocols. Let’s normalize recovery, not shame it.
Joe Jeter
January 1, 2026 AT 11:49Interesting how this post ignores the fact that many people use benzos to manage chronic pain, PTSD, or epilepsy-not just ‘anxiety’. Tapering them without alternatives is cruel. You don’t get to prescribe recovery like it’s a diet plan. Some of us are surviving, not thriving.
Usha Sundar
January 3, 2026 AT 10:43My mom tapered off in 6 months. She cried every night. Now she reads novels. No pills. No drama. Just quiet.
Isaac Bonillo Alcaina
January 5, 2026 AT 02:04Let’s be clear: this is not medical advice. It’s a marketing pamphlet disguised as a clinical guideline. The FDA didn’t ‘require’ label changes because benzos are dangerous-they did it because of litigation risk and political pressure. The 2024 guideline? A consensus of bureaucrats, not scientists. And ‘peer support’? That’s just group therapy with a new name. Don’t confuse community with competence.