- 8
Tacrolimus Neurotoxicity Risk Assessment Tool
Risk Assessment
When you’ve just had a transplant, the last thing you want is to feel like your body is betraying you. You’re taking tacrolimus to keep your new organ alive, but suddenly your hands won’t stop shaking. Your head pounds like it’s being squeezed in a vise. You can’t write your name, you can’t sleep, and your doctor says your blood levels are ‘in range.’ That’s when you realize: tacrolimus neurotoxicity isn’t just a footnote in a drug leaflet-it’s a real, disruptive, and often misunderstood side effect that affects up to 40% of transplant recipients.
What Tacrolimus Neurotoxicity Really Looks Like
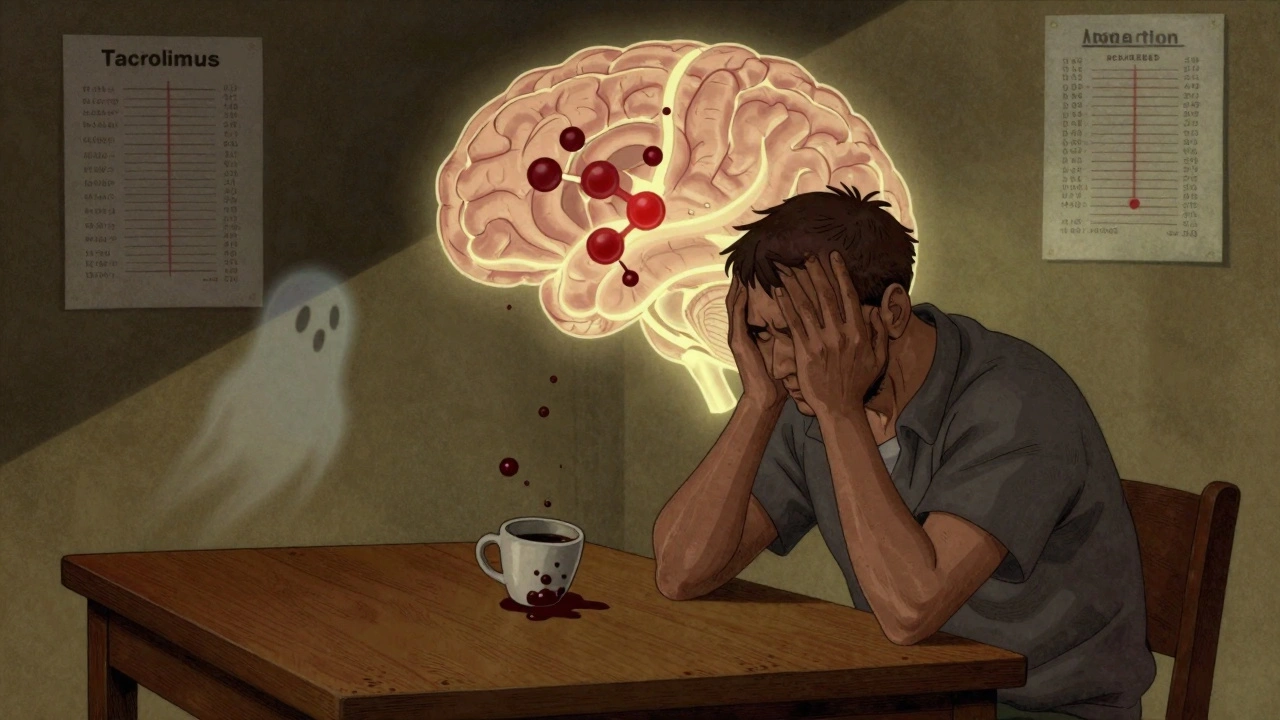
Tacrolimus is one of the most powerful immunosuppressants used after kidney, liver, heart, or lung transplants. It works by blocking calcineurin, a protein that tells your immune system to attack the new organ. But it doesn’t just target the immune system-it crosses the blood-brain barrier and messes with nerve cells. The result? Neurological symptoms that can range from annoying to terrifying.The most common sign? Tremor. About 65 to 75% of people who develop neurotoxicity report uncontrollable shaking, usually in the hands. It’s not like Parkinson’s tremor-it’s more like a fine, rapid vibration that makes holding a coffee cup impossible. Headache comes next, reported by nearly half of affected patients. These aren’t ordinary tension headaches. They’re often described as crushing, constant, and unresponsive to ibuprofen or acetaminophen.
Other symptoms include tingling in fingers or toes (paresthesia), trouble sleeping, dizziness, confusion, and in rare but serious cases, seizures or vision changes. One patient on a transplant forum described waking up unable to speak, then realizing she’d had a brief episode of speech arrest. Another said his vision doubled-like seeing two of everything-before he even realized it was a side effect.
What’s scary is that these symptoms can show up even when blood levels are perfectly within the ‘therapeutic’ range. A 2023 review in the Annals of Transplantation found that nearly one in five patients with neurotoxicity had tacrolimus levels below 15 ng/mL-the upper limit many doctors still consider safe. That means your numbers aren’t always the full story.
Why Blood Levels Don’t Tell the Whole Story
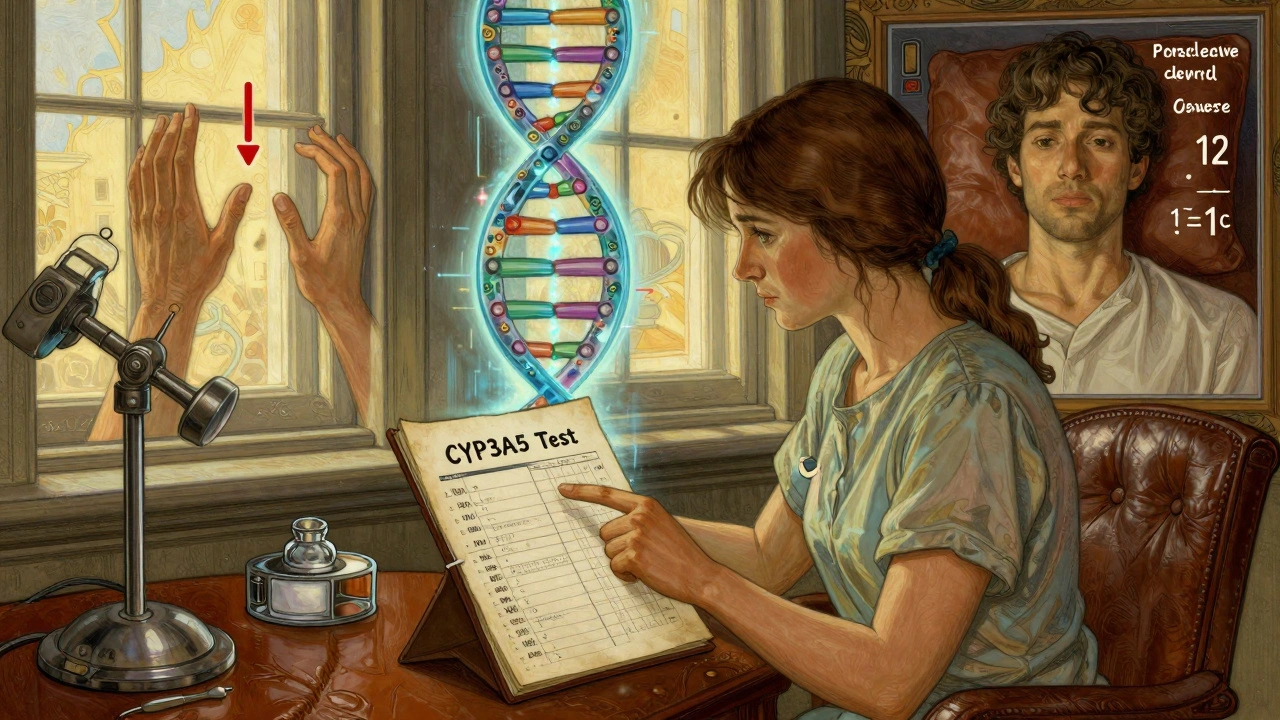
Doctors check tacrolimus blood levels because they’re supposed to be the guide. For kidney transplants, the target is usually 5-15 ng/mL. For liver and heart, it’s 5-10 ng/mL. But here’s the problem: those ranges were set based on rejection rates, not neurological side effects.Some people can tolerate 14 ng/mL without a single tremor. Others start shaking at 7 ng/mL. Why? Genetics. About 15-20% of people carry a variant of the CYP3A5 gene that makes them metabolize tacrolimus much faster. Their bodies clear the drug quickly, so they need higher doses to stay protected. But that also means their brain gets hit harder by peak concentrations. In a 2021 study from the University of Toronto, patients with this genetic profile had a 27% lower risk of neurotoxicity when dosed based on their CYP3A5 status instead of weight or standard protocols.
It’s not just genes. Electrolyte imbalances-especially low sodium (hyponatremia)-make neurotoxicity worse. A 2023 review found that correcting sodium levels alone resolved mild symptoms in nearly 30% of cases without changing the tacrolimus dose. Dehydration, diuretics, or even too much salt restriction can push you over the edge.
And then there are drug interactions. Antibiotics like linezolid, sedatives like midazolam, and even some antipsychotics can stack on top of tacrolimus and increase seizure risk. One patient developed a seizure after being given lorazepam for anxiety-something his transplant team hadn’t flagged as dangerous.
Who’s at Highest Risk?
Not everyone gets neurotoxicity. But some groups are far more likely to.Liver transplant recipients have the highest risk-around 35.7% in one major study. Kidney recipients are next at 22.4%, then lung at 18.9%, and heart at 15.2%. Why? It’s not entirely clear, but liver transplants often involve more complex blood flow changes, higher drug exposure, and more frequent use of other neurotoxic meds during surgery.
Age matters too. Older patients are more sensitive. So are people with pre-existing neurological conditions, like migraines or peripheral neuropathy. And if you’ve had a previous episode of neurotoxicity, you’re far more likely to get it again-even at lower doses.
One of the biggest red flags? Timing. Symptoms usually show up in the first 30 days after transplant, when drug levels are still being adjusted. That’s why the American Society of Transplantation now recommends routine neurological checks during this window. If you’re shaking, having headaches, or feeling ‘off,’ don’t wait for your next lab test. Tell your team right away.
What Happens When You Have Symptoms?
The first step is never to stop tacrolimus on your own. Without it, your body could reject the transplant within days. Instead, your care team will look at three things: your symptoms, your blood levels, and your overall health.If symptoms are mild-just a little tremor or occasional headache-they might lower your dose slightly. A reduction from 0.1 mg/kg to 0.07 mg/kg can be enough to calm symptoms while still protecting the organ. One patient on the National Kidney Foundation forum saw his tremor vanish in just 72 hours after a small dose drop.
If symptoms are moderate to severe-confusion, speech trouble, vision changes, or seizures-they’ll consider switching you to another immunosuppressant. Cyclosporine is the most common alternative. It’s less potent at preventing rejection, but it causes neurotoxicity about 15-20% less often. The trade-off? You’re more likely to have an acute rejection episode. Studies show rejection rates jump by 15-20% after switching.
Another option is switching to sirolimus or belatacept, which don’t affect calcineurin at all. But these drugs come with their own risks-higher chance of infection, slower wound healing, or lung issues. They’re usually reserved for people who can’t tolerate any calcineurin inhibitor.
In rare cases, if PRES (Posterior Reversible Encephalopathy Syndrome) is suspected-characterized by seizures, vision loss, and swelling in the back of the brain-an MRI is done immediately. Treatment involves stopping tacrolimus, controlling blood pressure, and sometimes using antiseizure meds. Most people recover fully if caught early.
What You Can Do Right Now
If you’re on tacrolimus, here’s what actually helps:- Track your symptoms daily. Keep a simple log: tremor? (yes/no), headache severity (1-10), sleep quality, dizziness. Bring it to every appointment.
- Ask about CYP3A5 testing. It’s not standard everywhere, but if your team hasn’t mentioned it, ask. It’s a simple blood or saliva test that can guide dosing.
- Check your sodium levels. If you’re on diuretics or drinking too little water, your sodium could be dropping. Ask for a basic metabolic panel every few weeks.
- Review all your meds. Tell every doctor you see that you’re on tacrolimus. Even a common antibiotic or sleep aid could be making things worse.
- Don’t ignore early signs. Tremor and headache aren’t ‘just part of recovery.’ They’re warning signs. Push for an evaluation if they persist beyond a few days.
One transplant nurse in Sydney told me: ‘The patients who survive best aren’t the ones with perfect labs. They’re the ones who speak up the moment something feels wrong.’
The Future: Personalized Dosing and New Drugs
The field is starting to change. The TACTIC trial, launched in 2024, is testing a new dosing algorithm that uses your CYP3A5 gene, your magnesium levels, and your blood pressure to predict your ideal tacrolimus dose-before symptoms start. Early results show it could cut neurotoxicity by more than half.Meanwhile, a new drug called LTV-1 is in phase 2 trials. It’s designed to work like tacrolimus but can’t cross the blood-brain barrier as easily. If it works, it could replace tacrolimus as the gold standard by 2027.
For now, tacrolimus remains the most effective tool we have to save transplanted organs. But its neurotoxicity isn’t a side effect we can ignore. It’s a signal-sometimes subtle, sometimes loud-that your brain is under stress. Recognizing it early, understanding your personal risk, and working with your team to adjust your plan can mean the difference between living with discomfort and living well.
Can tremor from tacrolimus go away on its own?
Yes, in many cases. Mild tremor often improves within days to a week after a small dose reduction or when electrolyte imbalances are corrected. However, if tremor worsens or is accompanied by confusion, vision changes, or seizures, it’s not something to wait out-medical intervention is needed immediately.
Is headache from tacrolimus dangerous?
Not always. Headaches are common and often mild. But if the headache is sudden, severe, unlike any you’ve had before, or comes with nausea, vision changes, or confusion, it could be a sign of PRES-a rare but serious brain condition. An MRI is needed to rule it out. Don’t assume it’s just a migraine.
Why do my tacrolimus levels seem fine but I still have symptoms?
Because blood levels don’t show how much drug is actually reaching your brain. Genetics, blood-brain barrier permeability, drug interactions, and electrolyte levels all play a role. Two people with the same blood level can have very different brain exposure. That’s why symptoms don’t always match lab numbers.
Should I get tested for CYP3A5 gene variants?
If you’ve had neurotoxic symptoms, or if you’re starting tacrolimus and have a history of sensitivity to medications, yes. CYP3A5 testing helps doctors tailor your dose to your body’s metabolism. It’s not routine everywhere, but it’s becoming more common in transplant centers. Ask your pharmacist or transplant team.
Can I switch to cyclosporine if tacrolimus causes too many side effects?
Yes, many patients do. Cyclosporine causes fewer neurological side effects but carries a higher risk of organ rejection and kidney damage. Your team will monitor you closely after the switch. It’s not a perfect solution, but for some, it’s the best way to balance safety and effectiveness.
How long does it take for neurotoxicity symptoms to resolve?
Most mild symptoms improve within 3 to 7 days after adjusting the dose or correcting electrolytes. Severe cases, like PRES, may take weeks to fully resolve, and some neurological changes can linger. But with timely intervention, full recovery is common.
Are there any long-term brain effects from tacrolimus neurotoxicity?
In most cases, no. Neurotoxicity from tacrolimus is usually reversible. However, untreated PRES or repeated episodes of severe neurotoxicity can rarely lead to permanent damage, like white matter changes or cognitive decline. That’s why early recognition and management are critical.
What’s Next?
If you’re on tacrolimus and have any neurological symptoms, don’t wait. Keep a symptom journal. Ask about CYP3A5 testing. Get your sodium checked. Talk to your pharmacist about every medication you’re taking-even over-the-counter ones. You’re not overreacting. You’re being proactive.The goal isn’t just to survive your transplant. It’s to live well after it. And that means paying attention to every signal your body sends-even the quiet ones.

val kendra
December 5, 2025 AT 13:08Been on tacrolimus for 3 years post-kidney transplant. Tremors started at 8 ng/mL. My doc said it was 'normal' until I brought up the CYP3A5 study. Got tested, turned out I'm a fast metabolizer. Dose dropped 20%, tremors gone in 72 hours. Stop letting labs dictate your quality of life.
Karl Barrett
December 6, 2025 AT 01:12It's fascinating how pharmacogenomics is finally creeping into transplant care. The CYP3A5 polymorphism isn't just a footnote-it's a paradigm shift. We've been treating tacrolimus like a one-size-fits-all blunt instrument when the brain's microenvironment responds to pharmacokinetic nuance. The blood level is a proxy, not a truth. What we're seeing is interindividual variability in blood-brain barrier permeability, modulated by inflammatory cytokines, electrolyte gradients, and even gut microbiome-derived metabolites. This isn't just neurotoxicity-it's a systems biology failure of our current dosing models.
Ben Choy
December 7, 2025 AT 16:13Thank you for this. I had PRES after my liver transplant. MRI showed swelling in the occipital lobe. They lowered my tacrolimus and gave me magnesium IV. Took 3 weeks to feel like myself again. Now I check my sodium every week. And I tell every new transplant patient I meet: if your head feels like it's in a vice, don't wait. Speak up. 🙏
Scott van Haastrecht
December 8, 2025 AT 02:23So you're telling me I shouldn't just trust my doctor's numbers? What a joke. My levels are perfect. I'm fine. Everyone else is just weak. You people act like a little tremor means you're dying. Get over it. I've been on this drug for 5 years. I'm still alive. That's all that matters.
Heidi Thomas
December 9, 2025 AT 11:21Anyone else notice how the article conveniently omits that tacrolimus is the only drug that keeps you alive? You want to switch to cyclosporine? Fine. Then your kidney fails and you're back on dialysis. You want to stop the drug? Great. Rejection kills faster than side effects. Stop whining and be grateful you're alive at all.
Libby Rees
December 9, 2025 AT 16:48I appreciate the thoroughness of this post. It is rare to encounter such a well-researched and clinically grounded perspective on post-transplant pharmacology. The emphasis on symptom tracking and electrolyte balance is particularly commendable. I would only add that patients should also consider monitoring serum magnesium levels, as hypomagnesemia can potentiate neurotoxic effects. A simple daily supplement may mitigate symptoms in some cases.
Emmanuel Peter
December 10, 2025 AT 22:45So you're saying I need a genetic test to know if I can tolerate a drug my doctor prescribed? That's ridiculous. You're just trying to make medicine more complicated so you can charge more. I'm not paying for a DNA test to stop my hands from shaking. Just give me a lower dose. Or better yet, stop prescribing this drug to people who can't handle it.
Jenny Rogers
December 11, 2025 AT 10:11It is both morally and scientifically indefensible to suggest that patients should adjust immunosuppressant dosing based on anecdotal experience or non-standardized biomarkers. The therapeutic window established by decades of clinical trials is not a suggestion-it is a standard of care. To prioritize subjective symptoms over objective lab values is to endanger not only the individual but the integrity of transplant medicine as a whole. One must ask: who is responsible for the inevitable rejection events that follow these reckless recommendations?