Safe Sleep Aid Use: What Works, What Risks, and How to Stay Protected
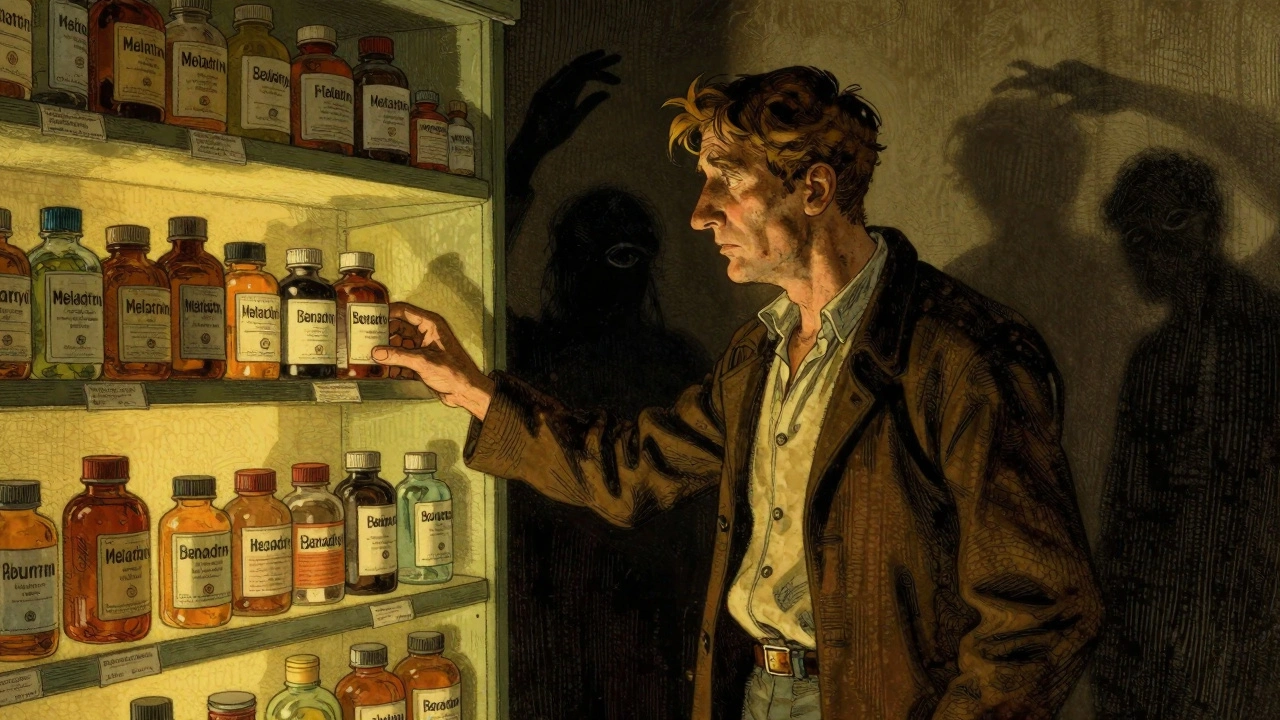
When you can’t sleep, a sleep aid might seem like the easiest fix—but safe sleep aid use, the practice of choosing and taking sleep medications without causing harm or dependency. Also known as responsible sleep medication use, it’s not just about popping a pill. It’s about understanding what’s in it, how it affects your body long-term, and whether your other health conditions make it risky. Many people assume over-the-counter or even prescription sleep aids are harmless because they’re widely available. But that’s not true. Even something as simple as diphenhydramine in Benadryl can leave you groggy all day, increase your fall risk, or worsen sleep apnea—especially if you’re over 65 or have heart or lung problems.
What makes sleep aids, medications or supplements used to induce or maintain sleep. Also known as hypnotics, they include both OTC options and prescription drugs like zolpidem or trazodone. dangerous isn’t always the drug itself—it’s how it interacts with what else you’re taking. For example, combining sleep aids with painkillers, antidepressants, or even certain antibiotics like ciprofloxacin can lead to extreme drowsiness, low blood pressure, or breathing problems. If you’re managing sleep apnea, a condition where breathing stops and starts during sleep, often linked to snoring and daytime fatigue. Also known as obstructive sleep apnea, it’s a major risk factor for heart disease and stroke., many sleep aids can make it worse by relaxing throat muscles too much. That’s why doctors often recommend treating the root cause—like weight loss or a CPAP machine—instead of just masking the symptom with a pill.
And then there’s the long game. Sleep aids don’t fix insomnia; they just cover it up. Over time, your body builds tolerance, meaning you need more to get the same effect. That’s when dependence kicks in—and quitting becomes harder than ever. Some people end up taking them for months or years without realizing they’ve lost the ability to sleep naturally. The real goal? Learn how to sleep better without pills. That means fixing your sleep schedule, cutting caffeine after noon, reducing screen time before bed, and managing stress. If you’re still struggling, talk to your doctor about cognitive behavioral therapy for insomnia (CBT-I)—it’s proven to work better than any medication in the long run.
What you’ll find here aren’t generic tips or marketing fluff. These are real, practical guides from people who’ve seen the consequences of unsafe sleep aid use—patients with liver disease who couldn’t metabolize common pills, older adults who fell after taking nighttime antihistamines, or people who didn’t know their snoring was a sign of something far more serious. We cover what to avoid, what to ask your pharmacist, how to read labels that hide dangerous interactions, and why sometimes, the safest sleep aid is no pill at all.