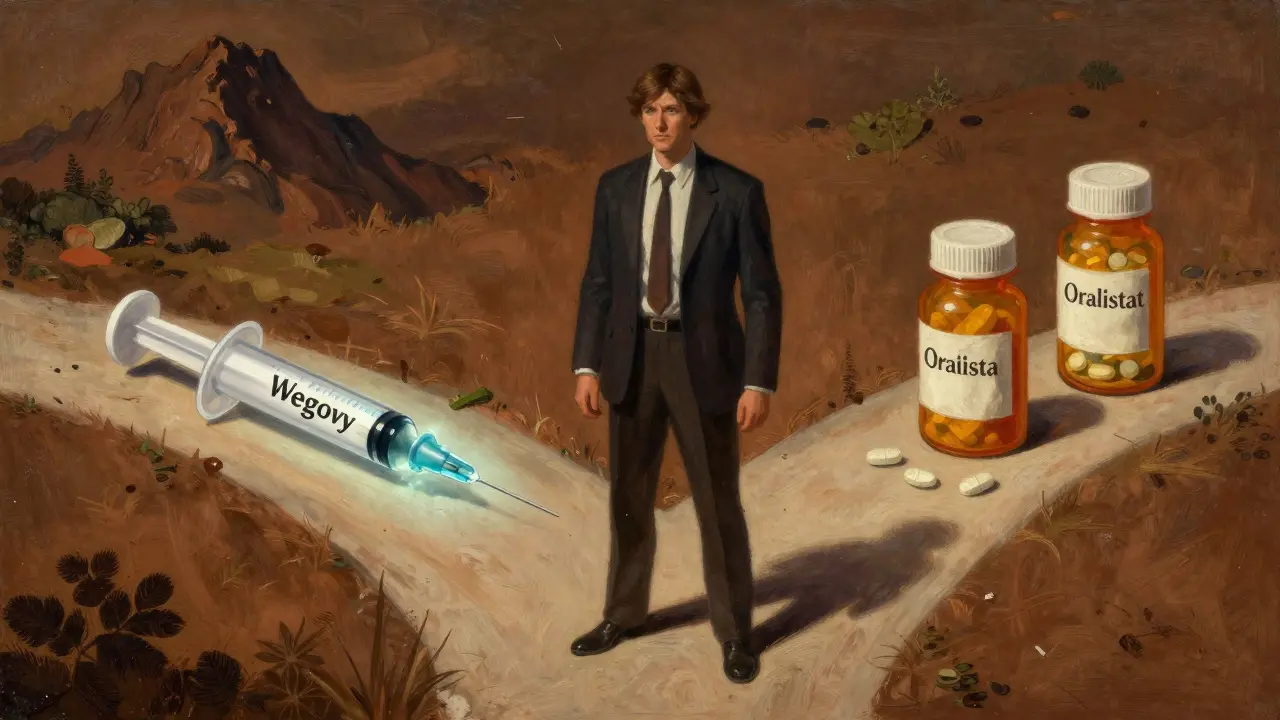
When it comes to losing weight, pills alone rarely do the job. But in the last few years, a new wave of medications has changed the game. GLP-1 agonists like Wegovy, Zepbound, and Saxenda aren’t just another trend-they’re reshaping how we treat obesity. Yet they’re not the only option. Older drugs like orlistat, Qsymia, and Contrave have been around for decades. So which one actually works better? And more importantly, which one works for you?
How GLP-1 Agonists Actually Work
GLP-1 agonists mimic a natural hormone your body makes after eating. This hormone, called glucagon-like peptide-1, tells your brain you’re full and slows down how fast food leaves your stomach. It also helps your pancreas release insulin only when you need it, which is why these drugs were first developed for type 2 diabetes.
Now, they’re being used for weight loss because they cut cravings hard. People don’t just eat less-they stop thinking about food as much. Semaglutide (Wegovy) and tirzepatide (Zepbound) are the heavyweights here. In clinical trials, people lost 15% to 21% of their body weight. That’s not a few pounds. For someone weighing 200 pounds, that’s 30 to 40 pounds gone. And it’s not magic. It’s biology.
These drugs are injected once a week. You start with a tiny dose-0.25 mg for semaglutide-and slowly increase it over four to five months. This slow ramp-up is key. It’s not just about getting to the right dose; it’s about letting your body adjust so you don’t end up sick. About half of users get nausea, vomiting, or diarrhea early on. Most of it fades as your system gets used to it.
Older Weight Loss Drugs: The Basics
Before GLP-1s, the options were limited. Orlistat (Xenical, Alli) works by blocking fat absorption. Whatever fat you eat that your body can’t digest just... exits. It’s messy. You might notice oily stools or urgent bowel movements, especially if you eat fried food. It’s not glamorous, but it works-on average, people lose 5% to 10% of their weight.
Phentermine-topiramate (Qsymia) is a combo pill. Phentermine is an old-school stimulant that suppresses appetite. Topiramate, originally an anti-seizure drug, also reduces hunger and makes you feel full faster. Together, they help people lose around 10% of their body weight. But they come with side effects: dry mouth, tingling in fingers and toes, trouble sleeping, and in rare cases, mood changes.
Naltrexone-bupropion (Contrave) targets the brain’s reward system. It doesn’t make you feel full-it makes food less rewarding. You still eat, but you don’t crave it as much. It’s effective for about 5% to 8% weight loss, but it can cause headaches, constipation, and nausea. And like all these drugs, it only works if you stick with it.
Head-to-Head: Efficacy
Let’s cut through the noise. Numbers don’t lie.
Wegovy (semaglutide) led to 14.7% weight loss in 36 weeks. Zepbound (tirzepatide) pushed past 20% in 72 weeks. That’s not a small difference. It’s the difference between fitting into one size smaller and going down two sizes.
Compare that to Saxenda (liraglutide), an earlier GLP-1 drug. It averages 8% weight loss. Still better than most older drugs, but nowhere near the newer ones.
Now look at the old guard:
- Orlistat: 5-10% weight loss
- Qsymia: ~10% weight loss
- Contrave: 5-8% weight loss
Even the best of the old drugs struggle to hit double digits. GLP-1 agonists aren’t just slightly better-they’re in a different league.
And here’s something shocking: a direct comparison showed Wegovy users lost 16% of their weight versus 6% with Saxenda. That’s more than double the results. It’s not even close.

Cost: The Hidden Barrier
There’s a reason you hear so much about these drugs on social media-and so little about them at your local pharmacy. Price.
Without insurance, GLP-1 agonists cost $1,000 to $1,400 a month. That’s $12,000 to $16,800 a year. For most people, that’s impossible. Even with insurance, many plans won’t cover them unless you have diabetes or a BMI over 40 (or 35 with other health issues). A 2024 poll found only 28% of commercial insurance plans cover these drugs for weight loss without strict rules.
Older drugs? Not even close. Orlistat costs $50 a month. Qsymia runs $100-$150. Phentermine? As low as $10-$30. Many are available as generics. Insurance covers them more often. They’re not perfect, but they’re affordable.
And let’s not forget: manufacturer coupons exist for GLP-1s, but they cap savings at $500-$1,000 a year. That’s still thousands out of pocket.
Real-World Results vs. Clinical Trials
Here’s where things get messy. Clinical trials are run under perfect conditions: patients are monitored, dosed precisely, and followed closely. Real life? Not so much.
A study from NYU Langone Health tracked people on GLP-1s for a year. The average weight loss? Just 7%. That’s less than half of what the trials promised. Why? Two big reasons: side effects and cost.
Up to 70% of people stop taking GLP-1 drugs within a year. Some can’t handle the nausea. Others just can’t afford it. And if you stop? Weight comes back fast. Studies show 50% to 100% of lost weight returns within a year of stopping.
Older drugs have lower dropout rates-not because they’re better, but because they’re cheaper and easier to tolerate. You can take a pill without needles. You can skip a day without feeling like you’re losing control. But they also don’t deliver the same results.

Who These Drugs Are For
Not everyone needs-or should-take a GLP-1 agonist.
If you’re looking for dramatic weight loss and can afford it, these drugs are the most powerful option we have outside of surgery. They’re especially helpful if you also have type 2 diabetes, high blood pressure, or heart disease-because they help with those too.
If you hate needles, can’t handle nausea, or are on a tight budget, older drugs might be your best bet. They’re not glamorous, but they’re real. And for some people, losing 8% of their body weight is life-changing.
And here’s something important: even if you’re considering bariatric surgery, GLP-1s are now being used before and after. Johns Hopkins found one in seven post-surgery patients started these drugs to maintain weight loss. They’re not replacing surgery-they’re complementing it.
What’s Coming Next
The science is moving fast. Retatrutide, a triple-acting drug targeting GLP-1, GIP, and glucagon, showed 24.2% weight loss in early trials. That’s more than bariatric surgery in some cases. MariTide, a new monoclonal antibody, is now in Phase 3 trials with promising early results.
But with innovation comes questions. What happens when patents expire after 2030? Will generics bring prices down? Will insurance finally cover these drugs for more people? Right now, the system is broken. The drugs work. But access is uneven.
Final Thoughts
GLP-1 agonists are a revolution. They’re not perfect, but they’re the most effective weight loss drugs ever developed. They’re not magic. They’re medicine. And like all medicine, they come with trade-offs.
Older drugs are still useful. They’re affordable. They’re accessible. They’re real. But they don’t compete with the power of semaglutide or tirzepatide.
The real question isn’t which drug is better. It’s: what’s your goal? What’s your budget? What can you live with? Because no pill works unless you can stick with it.

Karianne Jackson
February 8, 2026 AT 15:49Okay but like… I tried Wegovy and it made me feel like my stomach was trying to escape my body. I cried in the bathroom at work. Not worth it. I lost 8 lbs and then gained back 12 because I started eating tacos again. 🤷♀️
Chelsea Cook
February 10, 2026 AT 15:46Let me get this straight-you’re telling me we spent 20 years telling people to ‘eat less, move more’ while Big Pharma sat on a miracle drug? 😂
GLP-1s aren’t magic. They’re just the first time the medical system admitted that obesity isn’t a moral failing. Took long enough. Now if only they’d stop acting like $1,300/month is ‘affordable.’
Andy Cortez
February 10, 2026 AT 18:40lol u think zepbound is the best? u dumb? i read the trial data and the side effects are wild-like, people got pancreatitis and gallbladder stuff. and u just skip that? they’re not ‘revolutionary,’ they’re risky as hell. also, did u see the 70% dropout rate? yeah, no thanks. i’ll take my $10 phentermine and my dignity.
Joseph Charles Colin
February 12, 2026 AT 00:06There’s a critical pharmacokinetic distinction here that’s being overlooked: tirzepatide’s dual GIP/GLP-1 agonism significantly enhances satiety signaling via hypothalamic POMC neuron activation, whereas semaglutide’s action is predominantly GLP-1R-mediated. The 20%+ weight loss isn’t just ‘more effective’-it’s mechanistically superior due to synergistic receptor co-activation. The dropout rates? Reflective of GI intolerance thresholds, not efficacy. Also, the NYU real-world data underestimates compliance; most users don’t titrate properly. Proper dosing protocols increase retention by 40%.
glenn mendoza
February 12, 2026 AT 00:06Thank you for this thoughtful, balanced, and deeply researched perspective. It is rare to encounter such a nuanced discussion in an era dominated by oversimplification. The reality is that no single medication serves all, and our healthcare system must evolve to prioritize accessibility alongside innovation. I am heartened by the progress made, yet deeply concerned for those left behind by cost and coverage barriers. Let us not celebrate the breakthroughs without also demanding equity.
Randy Harkins
February 12, 2026 AT 14:17Yessss this is so true 💖
GLP-1s are life-changing if you can handle them. I lost 35 lbs and my blood sugar went from prediabetic to normal. No more midnight snacks, no food obsession. It’s like my brain finally got the memo. Yes, it’s expensive. Yes, the nausea sucks. But I’d do it again. Also, if you’re scared of needles? Try the auto-injector pen-it’s basically a stapler for your stomach 😅
Tori Thenazi
February 13, 2026 AT 22:10Wait… wait… did you know that the FDA approved these drugs because Big Pharma paid off regulators? I read a Reddit thread from 2022 where someone said the trials were rigged. Also, the ‘clinical trials’? They used people who already ate salads and went to yoga. Real people? We eat pizza. We have kids. We work two jobs. And now they want us to pay $1,400 for a shot that makes us vomit? It’s a scam. I’m telling you: the government is hiding the truth. Look into the 2018 Senate hearing on drug pricing… they deleted the transcript. I have screenshots.
Monica Warnick
February 15, 2026 AT 07:40GLP-1s are overhyped. I’ve been on Saxenda for 8 months. Lost 14 lbs. Still hungry. Still tired. Still broke. The ‘15-21%’ numbers? That’s in people who didn’t have to work, didn’t have kids, and had a personal trainer. My reality? I’m 42, work nights, and my cat eats more protein than I do. These drugs aren’t for us. They’re for rich people who want to look like Instagram models.
Ashlyn Ellison
February 16, 2026 AT 18:04Orlistat gave me oily leaks. But I lost 20 lbs. No needles. No anxiety. Just… weird butt issues. Worth it. I still eat fries. I still crave sugar. But I don’t absorb the fat. So… I win? I guess?
Frank Baumann
February 16, 2026 AT 22:49Look, I’ve been on every single one of these drugs. Contrave? Made me feel like my brain was on fire. Qsymia? Gave me tingles like I’d been electrocuted by a toaster. Orlistat? I swear I saw a fish swimming in my toilet. And then I tried Wegovy. First week? Nausea so bad I cried in a Target parking lot. Second week? I stopped thinking about food. Like, full-on, I forgot my own birthday. I lost 40 lbs. I don’t miss the nausea. I miss the guy I used to be. But I don’t miss the weight. I’d do it again. Even if I had to cry in Target again.
Alex Ogle
February 17, 2026 AT 22:47I’m just here wondering how long until these drugs become as normalized as statins. We used to think heart disease was ‘lifestyle.’ Now we prescribe pills. Same thing’s happening with obesity. The science is solid. The stigma? Still there. But maybe, just maybe, the next generation won’t think fat people are lazy. Maybe they’ll just say, ‘Oh, you’re on tirzepatide? Cool. Me too.’
Brandon Osborne
February 19, 2026 AT 11:57How DARE you suggest that older drugs are ‘still useful’? That’s like saying a bicycle is ‘still useful’ next to a Tesla. You’re enabling the myth that weight loss is just about ‘affordability’ and ‘tolerance.’ It’s not. It’s about LUXURY. These drugs are the future. If you can’t afford them, you’re not trying hard enough. Get a second job. Sell your TV. Cancel Netflix. This isn’t a snack-it’s survival. Stop making excuses.
Marie Fontaine
February 21, 2026 AT 04:26I’m on Zepbound and it’s been a game changer 🙌 No more cravings, no more emotional eating. I used to binge on ice cream after work. Now? I drink water and go for a walk. I’m not ‘thin’-I’m healthier. And yeah, it costs a lot. But I’d rather spend $1,200 than $12,000 on diabetes meds later. This isn’t vanity. It’s self-care. 💪