Chronic Alcohol Use Disorder isn’t just about drinking too much. It’s a medical condition where your brain and body become so dependent on alcohol that stopping feels impossible-even when it’s destroying your health, relationships, and life. This isn’t weakness. It’s a brain disease. And like any chronic illness, it needs real treatment, not judgment.
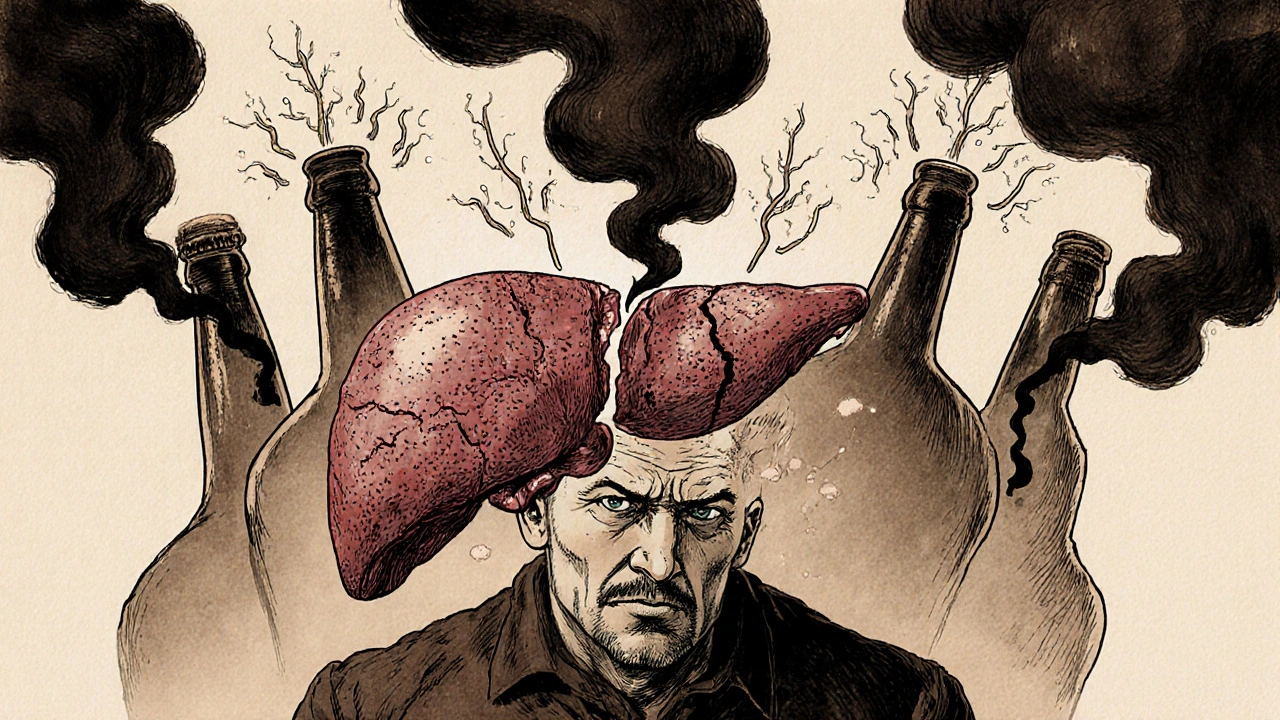
What Chronic Alcohol Use Disorder Actually Does to Your Body
Your liver doesn’t just get tired from drinking. It gets overwhelmed. After years of heavy use, 90% of people develop fatty liver-the first stage of alcohol-related liver damage. It’s reversible if you quit. But if you keep drinking, it turns into alcoholic hepatitis: inflamed, swollen liver cells dying off. Then comes cirrhosis-scar tissue replacing healthy tissue. Once cirrhosis sets in, your liver can’t filter toxins, make proteins, or store energy properly. Some damage can heal after stopping, but not all. The clock keeps ticking.
It’s not just your liver. Alcohol messes with your brain chemistry. Over time, your brain starts relying on alcohol to feel normal. When you stop, withdrawal hits hard: shaking, sweating, racing heart, confusion, even seizures. That’s not “being weak.” That’s your nervous system screaming for the chemical it’s been trained to expect.
Thiamine (vitamin B1) deficiency is common in people with long-term AUD. Up to 80% of those struggling with alcoholism lack it. That leads to Wernicke’s encephalopathy-a neurological emergency with confusion, loss of coordination, and abnormal eye movements. Left untreated, it can become Korsakoff syndrome: permanent memory loss, confabulation, and cognitive collapse.
Your heart isn’t safe either. Heavy drinking raises your risk of high blood pressure by 16%, increases your chance of atrial fibrillation by 40%, and boosts stroke risk by 34%. It weakens heart muscle, leading to cardiomyopathy. You don’t need to be a daily drinker to see this damage-binge drinking on weekends is enough to trigger irregular heart rhythms.
And your immune system? It’s down for the count. Alcoholics are 2.7 times more likely to get pneumonia. Your body can’t fight off infections the way it should. Even a simple cold can turn dangerous.
The Hidden Damage: Cancer, Mental Health, and More
Alcohol is a known carcinogen. It doesn’t just cause liver cancer. It raises your risk of mouth, throat, esophagus, breast, and bowel cancer. Heavy drinkers have five times the risk of mouth cancer. Just one drink a day increases breast cancer risk by 12%. There’s no safe threshold-only lower risk.
Alcohol doesn’t help depression. It makes it worse. It’s a depressant. It numbs emotions at first, but over time, it disrupts serotonin and dopamine. People with AUD are far more likely to have anxiety, depression, or suicidal thoughts. Many start drinking to cope-and end up trapped in a cycle that deepens the pain.
Relationships fall apart. Jobs are lost. Finances collapse. Homelessness becomes a real risk. The CDC says alcohol contributes to 29% of all traffic deaths in the U.S. It fuels violence, crime, and family breakdowns. The cost? $249 billion a year in the U.S. alone. Most of that comes from binge drinking-not daily heavy use.
How AUD Is Diagnosed (It’s Not What You Think)
There’s no blood test for alcohol use disorder. Diagnosis comes from behavior and symptoms. The DSM-5, the standard medical guide used by doctors worldwide, lists 11 criteria. If you meet two or more in a 12-month period, you have AUD. The severity is mild (2-3), moderate (4-5), or severe (6+).
Examples? You’ve tried to cut down and couldn’t. You spend a lot of time drinking or recovering. You keep drinking even though it’s hurting your health. You’ve given up activities you used to love. You need more alcohol to get the same effect. You get sick when you stop.
It’s not about how much you drink. It’s about control. Someone can drink a lot and not have AUD. Someone else drinks less but can’t stop when they want to. That’s the difference.

Treatment Isn’t One-Size-Fits-All
Detox is the first step-for people with physical dependence. It’s not optional. Quitting cold turkey can be deadly. Seizures, delirium tremens, heart failure-these are real risks. Medically supervised detox keeps you safe. Doctors use benzodiazepines to ease withdrawal symptoms and monitor vital signs.
After detox, recovery begins. Three FDA-approved medications help:
- Naltrexone blocks the pleasurable effects of alcohol. It reduces cravings. Taken as a daily pill or monthly shot (Vivitrol).
- Acamprosate helps stabilize brain chemistry after stopping. It reduces the urge to drink by calming overactive brain signals.
- Disulfiram makes drinking unpleasant. If you drink while on it, you get severe nausea, vomiting, and flushing. It’s a deterrent, not a cure.
Medication alone isn’t enough. It works best with therapy. Cognitive Behavioral Therapy (CBT) helps you spot triggers and build new habits. Studies show CBT reduces heavy drinking days by 60%. Motivational Enhancement Therapy (MET) helps you find your own reasons to quit-because you have to want it for yourself.
Support Groups: Real People, Real Results
Alcoholics Anonymous (AA) has been around since 1935. It’s free, everywhere, and based on peer support. Their 2014 survey found 27% of members stayed abstinent after one year. Critics say the numbers aren’t scientifically perfect-but the real test is in the lives changed. People show up, week after week. They get a sponsor. They work the steps. They find community.
Not everyone likes AA. That’s fine. There are alternatives: SMART Recovery (science-based, non-spiritual), Refuge Recovery (Buddhist-inspired), and Women for Sobriety. The goal isn’t the group-it’s the connection. Isolation fuels addiction. Connection fuels recovery.

New Treatments on the Horizon
Science is catching up. Transcranial Magnetic Stimulation (TMS), a non-invasive brain stimulation technique, showed 50% abstinence rates in a 2022 JAMA Psychiatry study. It targets the brain areas involved in cravings.
Digital tools are also helping. The reSET app, approved by the FDA, delivers CBT through your phone. In clinical trials, users were twice as likely to stay sober compared to those without it.
The MATTERS study proved something critical: combining medication with therapy increases abstinence by 24% compared to either alone. This isn’t theory-it’s practice. Treatment works best when it’s layered.
Recovery Is Possible-But It Takes Time
Some liver damage can reverse. Brain function can improve. Cravings fade. Relationships can mend. But recovery isn’t a quick fix. It’s a daily choice. Relapse is common. That doesn’t mean failure. It means the treatment needs adjusting.
Many people don’t get help. Only 19.2% of Americans with AUD receive treatment. Barriers? Cost. Shame. Lack of access. Misunderstanding. Too many still see AUD as a moral issue, not a medical one.
It’s not about willpower. It’s about biology. Your brain changed. Healing takes time, support, and the right tools. You don’t have to do it alone.
Where to Start
If you’re reading this and wondering if it’s about you-here’s what to do next:
- Talk to your doctor. No judgment. Just facts. Ask about AUD screening.
- Call a helpline. In Australia, Lifeline (13 11 14) or Alcohol and Drug Information Service (ADIS, 1800 250 015) offer free, confidential support.
- Consider a detox program. Don’t try to quit alone if you’ve been drinking heavily for months or years.
- Find a therapy option that fits you-CBT, MET, or a support group.
- Be patient. Recovery isn’t linear. Progress matters more than perfection.
You’re not broken. You’re sick. And like any illness, it can be treated. The sooner you act, the more your body and mind can heal.
Is chronic alcohol use disorder the same as alcoholism?
Yes, alcoholism is the common term for severe alcohol use disorder. The medical term changed in 2013 when the DSM-5 combined alcohol abuse and dependence into one diagnosis called alcohol use disorder (AUD). AUD has three levels: mild, moderate, and severe. Alcoholism usually refers to the severe form, where physical dependence and loss of control are clear.
Can you recover from liver damage caused by alcohol?
It depends. Fatty liver and early inflammation (alcoholic hepatitis) can reverse completely if you stop drinking. But once cirrhosis-permanent scarring-sets in, the damage can’t be undone. However, stopping alcohol can stop further damage and even improve liver function. Some people with cirrhosis live for years without needing a transplant if they stay sober.
Do I need medication to quit drinking?
Not everyone does, but it helps. Medications like naltrexone, acamprosate, and disulfiram reduce cravings and lower relapse risk. They work best with therapy. If you’ve tried quitting before and failed, medication might be the missing piece. Talk to your doctor-it’s not a sign of weakness. It’s smart medicine.
How long does alcohol withdrawal last?
Symptoms start within hours after your last drink. Peak intensity is usually between 24 and 72 hours. Physical symptoms like shaking and nausea often fade within a week. But psychological symptoms-anxiety, insomnia, cravings-can last weeks or months. That’s why ongoing support matters. Withdrawal is just the first step.
Is moderate drinking safe if I have AUD?
No. For someone with chronic alcohol use disorder, moderation is not a realistic goal. Your brain has changed. Even one drink can trigger a full relapse. Abstinence is the only proven path to recovery for severe AUD. The idea of “controlled drinking” works for some with mild AUD-but not for those with long-term dependence. It’s too risky.
What if I relapse after quitting?
Relapse doesn’t mean you failed. It means the treatment plan needs adjusting. Most people with chronic conditions like AUD experience setbacks. The key is to get back on track quickly. Call your counselor. Reconnect with your support group. Don’t wait until you’re back in full-blown use. Early intervention saves lives.
Are there any new treatments I should know about?
Yes. Transcranial Magnetic Stimulation (TMS) targets brain areas linked to cravings and has shown 50% abstinence rates in trials. Digital apps like reSET deliver CBT through your phone and have doubled abstinence rates in studies. The MATTERS study showed combining medication with therapy boosts success by 24%. These aren’t experimental-they’re available now, just not widely promoted.

Brian Bell
November 15, 2025 AT 15:56Man, this post hit different. I used to think drinking a six-pack on weekends was fine until my liver enzymes went through the roof. Now I’m 18 months sober and my brain feels like it finally stopped screaming. No magic pills, just time and showing up.
Sean Evans
November 15, 2025 AT 22:17Wow, another ‘alcoholism is a disease’ sermon. Let me guess-you’ve never met someone who just needed to grow a spine? My uncle drank for 30 years, lost his job, his wife, his kids-and still blamed ‘brain chemistry.’ Nah. He chose to keep drinking. No amount of neuroscience excuses laziness and selfishness. 🤷♂️
Scarlett Walker
November 16, 2025 AT 06:14Sean, I hear you-but you’re missing the point. This isn’t about blame. It’s about healing. My sister went through detox last year. She cried every night for weeks. But now? She’s back at her kid’s soccer games. She’s got a job. She’s alive. That’s not weakness. That’s courage. 💪❤️
Ashley Durance
November 16, 2025 AT 19:41Let’s be real: 90% of people with AUD are middle-aged white men who blame the system. The data shows binge drinkers-often college kids and young adults-are the real drivers of cost and harm. Why are we treating this like a chronic illness when it’s often just poor life choices wrapped in medical jargon?
Ryan Anderson
November 17, 2025 AT 19:44There’s a huge difference between ‘poor choices’ and neurobiological adaptation. The brain literally rewires itself. You can’t ‘just stop’ when your amygdala is screaming for alcohol like it’s oxygen. This isn’t about blame-it’s about biology. And biology deserves treatment, not judgment. 🙏
Anjan Patel
November 19, 2025 AT 01:19Ohhh my GOD!! This is the most important thing I’ve read in 10 years!! I’ve been drinking since I was 16!! My liver is screaming!! My wife left me!! My daughter doesn’t recognize me!! But now-I’m going to stop!! I’m going to do TMS!! I’m going to get Vivitrol!! I’m going to cry in AA until I’m healed!! 🌈✨🙏
Hrudananda Rath
November 20, 2025 AT 02:20One must observe with scholarly detachment that the conflation of ‘alcoholism’ with ‘brain disease’ represents a dangerous medicalization of moral failure. The DSM-5, a product of pharmaceutical-influenced consensus, has erased the concept of personal responsibility under the guise of compassion. One cannot cure vice with pharmacology.
Scott Saleska
November 20, 2025 AT 20:13Hey, I’m curious-have any of you tried the reSET app? I’ve been using it for 6 months. It’s not perfect, but it reminds me to breathe when I feel the urge. Also, my therapist said CBT + naltrexone cut my cravings by like 70%. Just saying. No pressure. Just… maybe it helps?
Kevin Wagner
November 21, 2025 AT 10:36Y’all are overcomplicating this. It’s simple: you drink too much, you get sick. You stop drinking, you get better. No magic. No mysticism. No guilt trips. Just quit. And if you can’t? Then you ain’t ready. No shame in that-just don’t pretend it’s a disease so you don’t have to face the truth. I’ve seen it a hundred times.
gent wood
November 21, 2025 AT 19:27I’ve worked in addiction services for 18 years. The most powerful thing I’ve ever seen isn’t medication or apps-it’s someone showing up, week after week, to a room full of strangers who don’t judge them. That’s the real medicine. Connection. Not chemicals. Not slogans. Just presence.
Eleanora Keene
November 23, 2025 AT 14:32im not a doctor but i think this is so important. my bro relapsed 3 times before he finally stuck with it. the first time he tried quitting he thought he could just drink less. big mistake. now he goes to meetings and does yoga and says his brain feels ‘quieter’. i just wish more people knew this stuff before it was too late. you got this. 💕
Nathan Hsu
November 25, 2025 AT 11:55Let me tell you about my cousin in Mumbai-he stopped drinking cold turkey after his father died, no meds, no therapy, just willpower. He’s been sober for 12 years. He works as a mechanic. He’s happy. He’s alive. The West over-medicalizes everything. Sometimes, the answer is just… stop.
Joe Goodrow
November 26, 2025 AT 17:30Why are we spending $249 billion on this? We’ve got real problems-border security, inflation, crime. Alcoholism? That’s a personal failing. If you can’t control your drinking, maybe you shouldn’t be allowed to drive, vote, or own a gun. This isn’t healthcare-it’s a welfare handout to people who refuse to grow up.
Ryan Anderson
November 27, 2025 AT 21:45Joe, I get your frustration. But that $249 billion? A huge chunk is from ER visits, car crashes, lost wages, and child services. That’s not just ‘personal failure’-that’s societal cost. And if we treat this like a disease, we save money long-term. Prevention beats incarceration. Compassion beats contempt. And yeah-sometimes, people need help to get strong.