Tacrolimus Blood Levels: What You Need to Know About Monitoring and Safety
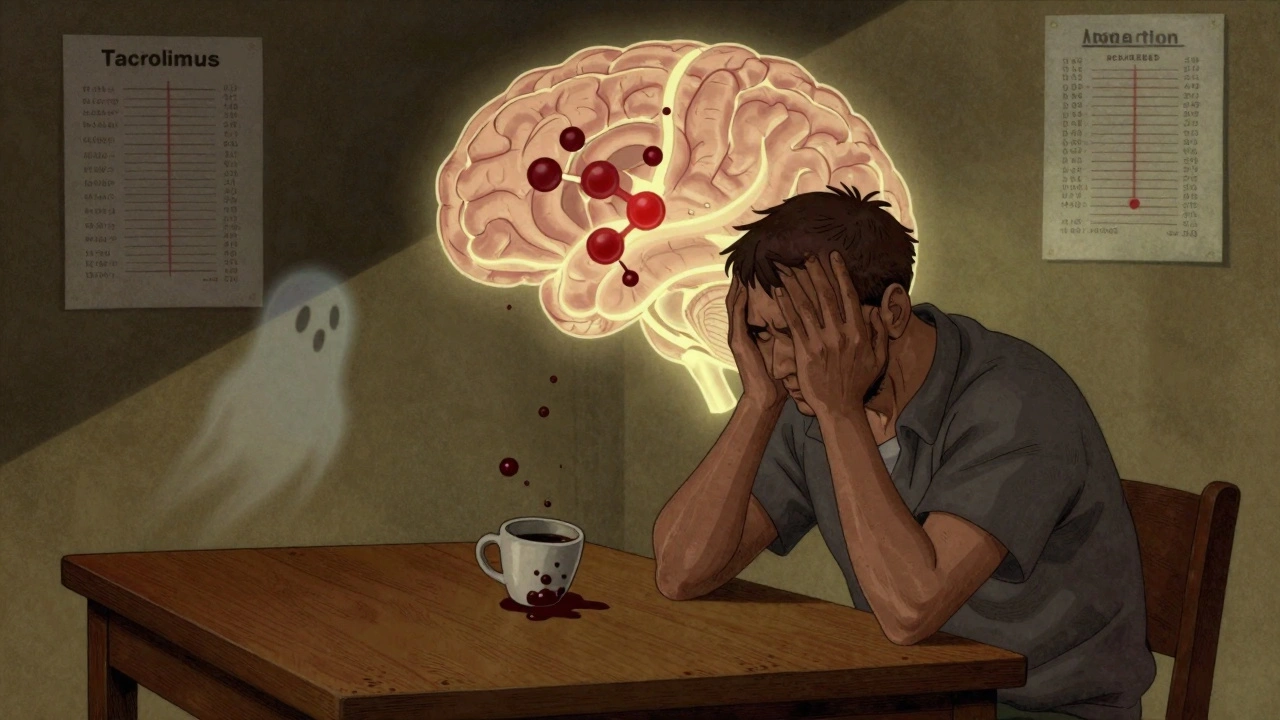
When you’re on tacrolimus, a powerful immunosuppressant used mainly after organ transplants to prevent rejection. Also known as FK506, it’s a drug that needs careful tracking because the difference between working and causing harm is often just a few nanograms per milliliter. Too little, and your body might attack the new organ. Too much, and you risk kidney damage, nerve problems, or even seizures. That’s why therapeutic drug monitoring, the process of regularly testing blood levels to keep medication within a safe range isn’t optional—it’s life-saving.
Tacrolimus doesn’t work the same way for everyone. Your liver’s ability to break it down, what other meds you’re taking, even what you ate that day can swing your levels up or down. For example, antibiotics like erythromycin, can slow down how fast your body clears tacrolimus, causing dangerous spikes. On the flip side, St. John’s wort or certain seizure meds can make tacrolimus disappear from your system too fast. And if you’ve got kidney disease, your body can’t filter the drug properly, making levels harder to control. That’s why doctors don’t just pick a number and call it good—they adjust based on your labs, symptoms, and history.
Most transplant centers aim for tacrolimus blood levels between 5 and 15 ng/mL in the first few months after surgery, then slowly lower it over time. But those numbers aren’t universal. A liver transplant patient might need higher levels than someone with a kidney transplant. And if you’ve had rejection before, your target might be pushed higher. The goal isn’t just to stay alive—it’s to stay well. That’s why you’ll see blood tests every week at first, then every few weeks, and eventually monthly. Skipping a test isn’t just risky—it’s like driving blindfolded.
Below, you’ll find real-world posts that connect the dots between tacrolimus and the bigger picture: how other drugs interfere, why comorbidities make dosing trickier, and how simple mistakes can lead to serious consequences. These aren’t theoretical guides—they’re based on what’s happening in clinics and pharmacies right now. Whether you’re a patient, caregiver, or just trying to understand why your lab results keep changing, this collection gives you the facts you need to ask the right questions and stay safe.