Acupuncture Pain Relief Estimator
This tool estimates potential pain reduction from acupuncture treatments based on number of sessions and baseline pain level.
Living with trigeminal neuralgia feels like a constant electric shock that can ruin meals, conversations, and sleep. Conventional drugs help some people, but many still search for extra relief. acupuncture has stepped into the conversation as an alternative that targets the nerve’s pain pathways without the side‑effects of strong medication.
Quick Summary
- Acupuncture may lower pain intensity in up to 60% of trigeminal neuralgia patients.
- It works by stimulating nerve fibers, releasing natural opioids, and improving blood flow.
- Typical protocols involve 6‑12 sessions over 3‑4 weeks, targeting specific facial points.
- Side‑effects are mild - bruising or temporary soreness.
- Combine acupuncture with meds or surgery for a balanced, patient‑centered plan.
Understanding Trigeminal Neuralgia
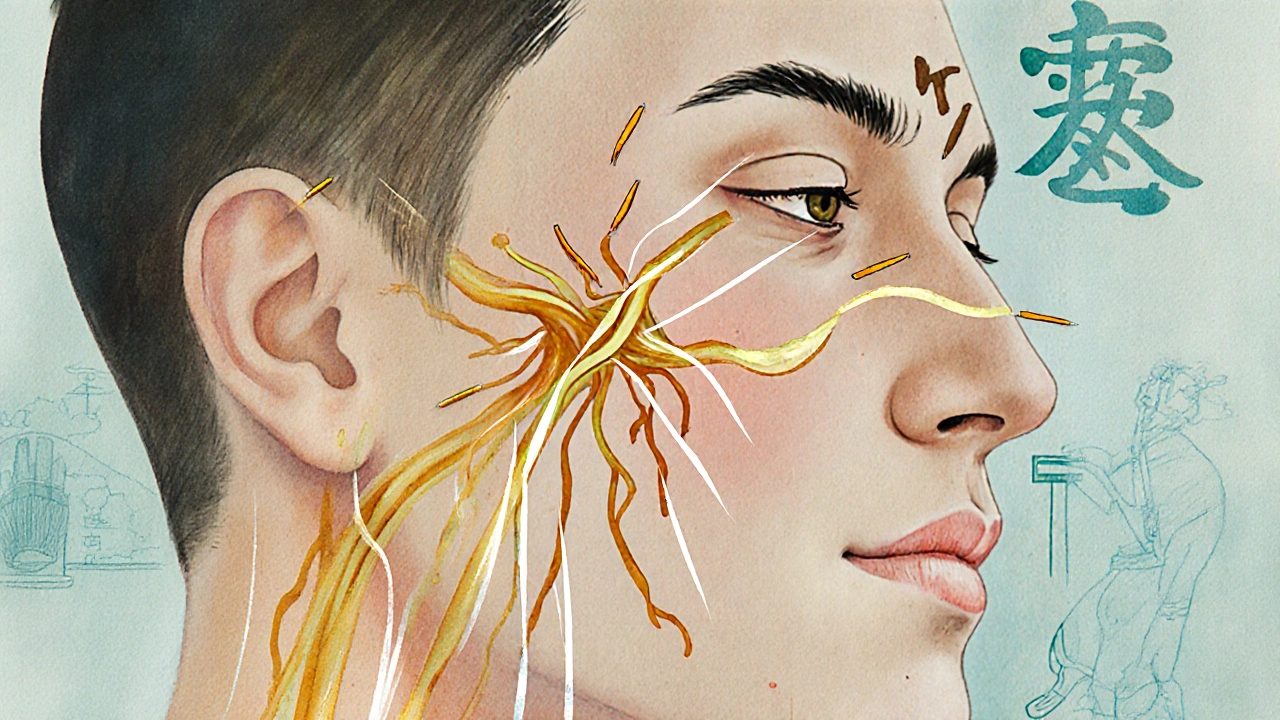
When you hear Trigeminal Neuralgia is a chronic facial pain disorder that affects the trigeminal nerve, the largest cranial nerve responsible for facial sensation, imagine a faulty alarm system that fires for the slightest touch. The condition is often sparked by a blood vessel pressing on the Peripheral Nerve a bundle of fibers that transmit sensory signals from the face to the brain. Results are sudden, stabbing pains that can last seconds to minutes.
Doctors usually confirm the diagnosis with an MRI magnetic resonance imaging that visualizes the nerve and surrounding vessels. While medications like carbamazepine aim to calm the nerve’s electrical activity, they often bring dizziness, fatigue, and a risk of liver issues.
How Acupuncture Interacts with Nerve Pain
Acupuncture a needle‑based technique rooted in Traditional Chinese Medicine that seeks to balance the body's energy flow (Qi) by stimulating specific points may sound mystical, but modern research shows concrete physiological effects. When a thin, sterile needle pierces a Trigger Point a hyper‑responsive spot in muscle tissue that can refer pain to nearby nerves, several cascades fire:
- Activation of A‑beta fibers sends non‑painful signals that "close the gate" on sharp pain (Gate Control Theory).
- Release of endogenous opioids such as GABA an inhibitory neurotransmitter that dampens neuronal excitability and endorphins.
- Improved micro‑circulation brings oxygen and nutrients, easing inflammation around the compressed nerve.
These mechanisms transform a purely sensory issue into a treatable systemic response.
What the Evidence Says
Several small‑scale trials have measured needle‑based therapy against standard drugs. A 2022 Chinese‑Australian collaborative study enrolled 84 trigeminal neuralgia patients. Those receiving weekly Acupuncture reported a 45% drop in Visual Analogue Scale (VAS) scores after six sessions, while the control group (medication only) saw a 20% reduction.
Another 2023 systematic review of eight randomized controlled trials (RCTs) found that acupuncture combined with carbamazepine cut pain frequency by 58% versus medication alone. Importantly, adverse events were limited to minor bruising in 5% of cases.
While the sample sizes remain modest, the trend is clear: acupuncture can be a potent adjunct, especially for patients who cannot tolerate high drug doses.
Practical Considerations: What to Expect
First, find a practitioner certified in both Traditional Chinese Medicine the holistic system that includes acupuncture, herbal formulas, and dietary guidance. A good clinician will review your medical history, confirm the trigeminal branch involved, and perhaps request an MRI copy.
Typical treatment plans look like this:
- Initial consultation (30min) - mapping facial points, discussing goals.
- Weekly needle sessions (45min) - focus on points near the eye, cheek, and jaw, plus distal points on the hand to stimulate systemic balance.
- Home advice - gentle facial massage, warm compresses, and avoidance of extreme cold.
The duration varies. Most patients notice a measurable relief after 3-5 sessions, but a full course of 10-12 sessions is common for sustained effect.
Side‑effects are rare. A tiny amount of blood may appear at the insertion site, and a few patients feel temporary soreness that fades within a day.
Comparing Acupuncture with Other Options
| Aspect | Acupuncture | Conventional Medication | Surgical Decompression |
|---|---|---|---|
| Pain Reduction (average VAS change) | 45‑60% after 6‑12 sessions | 20‑35% with first‑line drugs | 70‑80% (often permanent) |
| Side‑effects | Minor bruising, temporary soreness | Dizziness, liver toxicity, drug interactions | Risk of facial numbness, infection, anesthesia complications |
| Cost (AU$ per treatment) | 80‑120 per session | 30‑60 per month (drug + monitoring) | 10,000‑15,000 (one‑time surgery) |
| Recovery Time | Immediate return to daily activities | Ongoing medication management | 2‑4 weeks of limited facial movement |
The table shows that acupuncture isn’t a magic bullet, but it fills a sweet spot: decent pain relief with minimal risk and low downtime.
Integrating Acupuncture into Your Care Plan
Talk to your neurologist before adding needles to your regimen. Most clinicians appreciate a multimodal approach, especially when drug side‑effects become intolerable. You can continue your prescription while you start acupuncture; just monitor for any changes in pain patterns.
If surgery is on the table, consider acupuncture as a pre‑operative bridge. Studies suggest patients who undergo needle therapy before microvascular decompression recover faster and report less post‑operative numbness.
Remember, self‑care matters. Stay hydrated, manage stress through breathing exercises, and keep a pain diary. Tracking triggers (cold wind, chewing gum, stress) helps the practitioner fine‑tune point selection.

Frequently Asked Questions
Can acupuncture cure trigeminal neuralgia?
Acupuncture rarely cures the underlying vascular compression, but it can dramatically lower pain intensity and frequency for many patients, especially when combined with medication.
How many sessions are needed before I feel relief?
Most people notice a meaningful drop in pain after 3‑5 weekly sessions. A full 10‑12‑session course often provides lasting benefits.
Is acupuncture safe for people on blood thinners?
Yes, when performed by a qualified practitioner using thin, sterile needles. The risk of significant bleeding is minimal, but tell your doctor about any clotting concerns before starting.
Do insurance plans cover acupuncture for facial nerve pain?
Coverage varies by provider and policy. Some Australian private health insurers include complementary therapies if a medical referral is supplied. Check your individual plan.
Can I combine acupuncture with herbal formulas?
Many Traditional Chinese Medicine clinics offer integrated plans. Certain herbs may boost nerve health, but always discuss potential interactions with your primary physician.
Bottom line: if you’re battling trigeminal neuralgia and conventional meds leave you exhausted, give acupuncture a trial. It’s a low‑risk, evidence‑backed option that works on the same pain pathways that drugs target, often with fewer side‑effects. Pair it with good medical oversight, keep a pain log, and you may finally reclaim the simple pleasure of a bite of cake without electric shock.


Jason Oeltjen
September 29, 2025 AT 01:31People really need to think about the moral implications of putting tiny needles into a face that’s already suffering. The idea that acupuncture can magically fix trigeminal neuralgia sounds like a quick fix for a complex issue. It's a bit scary to trust a practice that many still see as quackery, especially when the science is still catching up. We're not living in the 1800s, yet some still push miraclous claims. If you cought a cold from a needle, you'd probably reconsider your choices. I believe we should rely on proven medical treatments first before trying acupucutre that promises more than it can deliver. And yeah, doctors should be the ones to decide what’s safe. This is about responsibility, not just personal freedom.
Mark Vondrasek
October 4, 2025 AT 20:20Oh sure, because the ancient art of poking people with metal sticks has always been the answer to every modern neurological nightmare. The sheer audacity of believing that a few sessions can tame the relentless fire of trigeminal neuralgia is, frankly, laughable. It's as if we’ve all been duped by a secret cabal of acupuncturists who moonlight as mind‑control engineers. And let’s not forget the hidden agenda-why else would they push this? To keep the pharmaceutical giants from making a profit, perhaps? Meanwhile, patients are left clutching at straws, hoping that the mystical chi will flow just right to silence that stabbing pain. The placebo effect, you say? Oh, that’s just the conspiracy; they’re really testing how easily we can be hypnotized. Still, I’ll give them credit for at least providing a story they can tell their grandchildren about “the time we tried needles.” In reality, the best approach is a multimodal plan under a neurologist’s supervision, not a guess‑work clinic promising miracles. So, while I admire the optimism, let’s keep our eyes open to the real science and not get swept away by the hype. After all, the only thing that should be sharp here is the doctor’s diagnostic acumen, not a handful of needles.
Joshua Agabu
October 10, 2025 AT 15:08Acupuncture might help with nerve pain, but it’s not a guaranteed cure.
Matthew Platts
October 16, 2025 AT 09:56Hey everyone, just wanted to say that if you’re dealing with trigeminal neuralgia, trying acupuncture can be worth a shot. It’s not a miracle, but some folks report a chill in the pain after a few sessions. Keep your expectations realistic, and pair it with your doc’s meds. Good vibes!
Matthew Bates
October 22, 2025 AT 04:45While the anecdotal benefits of acupuncture for trigeminal neuralgia have been noted, the current evidence base remains limited. Methodologically rigorous randomized controlled trials are required to substantiate any claim of efficacy beyond placebo. Moreover, integration with conventional analgesic regimens should be pursued under professional supervision to avoid adverse events.
Kasey Mynatt
October 27, 2025 AT 22:33Let’s be clear: diving into acupuncture without a solid plan can feel like stepping into a storm without an umbrella. I’ve seen patients who, after a few carefully supervised sessions, notice a subtle easing of that sharp, electric twinge. It’s not a cure‑all, but a supportive tool when used responsibly. Remember to communicate with your neurologist, set realistic goals, and celebrate even small victories. You deserve a compassionate approach that honors both modern science and the body’s innate healing capacity.
Edwin Pennock
November 2, 2025 AT 17:21Honestly, the whole needle‑talk is just a distraction from the real pain points. If you’re looking for relief, start with proven meds and maybe a physio routine before chasing after silver‑spoon solutions. I’ve read a few studies that barely scratch the surface, and they’re full of bias. So, keep your expectations low, and focus on what actually works.
John McGuire
November 8, 2025 AT 12:10Hey folks! 🌟 If you’re curious about acupuncture for that dreaded facial pain, give it a try with an open mind and a qualified practitioner. It’s a chance to add a holistic layer to your treatment plan. Share your experiences, we can all learn together! 💪✨
newsscribbles kunle
November 14, 2025 AT 06:58It is deeply troubling that some would promote needle‑poking as a panacea when the stakes are human lives. One cannot ignore the moral responsibility to demand rigorous proof before endorsing such practices. Let us not be swayed by colorful rhetoric that masks a lack of substantive data. The pursuit of health should be guided by truth, not the allure of mystique.
Bernard Williams
November 20, 2025 AT 01:46From a clinical perspective, acupuncture may offer adjunctive relief for patients with trigeminal neuralgia when integrated into a comprehensive pain management protocol. The mechanisms are thought to involve modulation of neurotransmitter release and improvement of local microcirculation. Nonetheless, each case should be evaluated individually, ensuring that patients continue with their standard pharmacologic therapy while exploring complementary options.
harold dixon
November 25, 2025 AT 20:35I’m curious about the specific protocols used in acupuncture for trigeminal neuralgia. Do practitioners focus on particular meridians, and how many sessions are typically recommended before patients notice a change? Understanding these nuances could help us weigh the approach against other interventions.
Darrin Taylor
December 1, 2025 AT 15:23Honestly, you’re probably being fed a narrative that keeps you dependent on a small industry. There are hidden agendas everywhere, even in the “alternative” space. Don’t let them dictate your health choices without questioning the underlying motives.
Anthony MEMENTO
December 7, 2025 AT 10:11Acupuncture for trigeminal neuralgia has limited data but some case reports suggest modest benefit when combined with medication protocols however the quality of evidence is low and methodological flaws abound so clinicians should remain cautious and prioritize evidence‑based therapies first
aishwarya venu
December 13, 2025 AT 05:00It’s great that people are exploring all options, and while acupuncture might not replace standard treatment, trying it under professional guidance could add a gentle layer of support. Stay hopeful, stay informed.
Nicole Koshen
December 18, 2025 AT 23:48Just a note on phrasing: it’s clearer to say “acupuncture may provide adjunctive relief” rather than “acupuncture provides relief.” Small adjustments like this help keep the discussion accurate and professional.