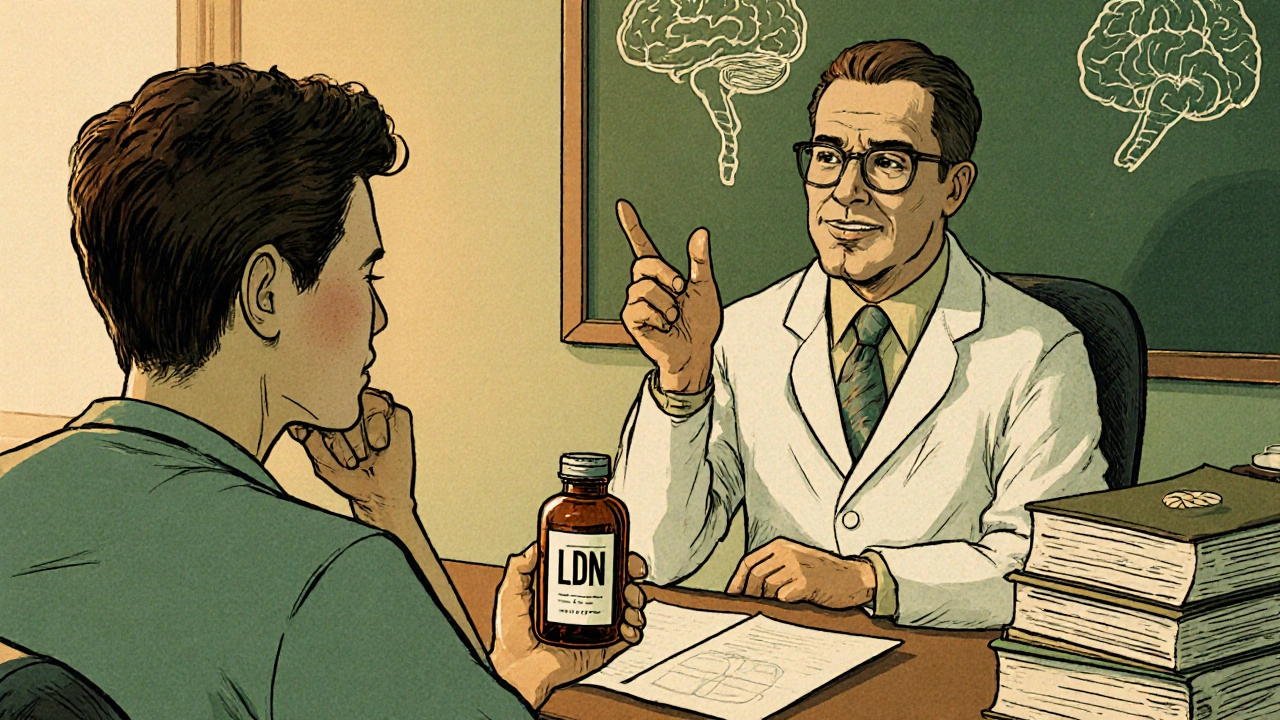
Ever wonder whether the buzz around Low Dose Naltrexone (LDN) is justified, or if there’s a better option for your chronic condition? You’re not alone. Many patients and clinicians are weighing LDN against a handful of off‑label and FDA‑approved drugs, trying to pin down which one actually delivers the relief they need.
What is Low Dose Naltrexone?
Low Dose Naltrexone is a low‑strength formulation of the opioid antagonist naltrexone, typically dosed between 1 mg and 4.5 mg per day. Unlike the standard 50 mg dose used for opioid or alcohol dependence, LDN is prescribed off‑label for its immunomodulatory and anti‑inflammatory effects.
How LDN Works - The Mechanism in Plain Speak
The short story: at low doses, naltrexone briefly blocks the body's opioid receptors, prompting a rebound surge in endogenous opioids like endorphins. This spike can reset the immune system, reduce inflammation, and ease pain. Think of it as a brief “reset button” for the opioid system, which then over‑compensates in a beneficial way.
Common Conditions Treated with LDN
Patients report improvement in a surprising range of ailments, including:
- Multiple sclerosis (MS)
- Fibromyalgia
- Crohn’s disease and ulcerative colitis
- Chronic fatigue syndrome
- Some cancers (as an adjunct therapy)
Because the evidence is largely anecdotal or from small trials, LDN remains a gray‑area treatment that hinges on individual response.
Alternatives to LDN - A Quick Rundown
Below are the most talked‑about substitutes, each with its own pros and cons.
Naloxone is an opioid antagonist similar to naltrexone but typically used in emergency overdose situations. In low doses, it may share some immunomodulatory properties, though data are sparse.
Buprenorphine is a partial opioid agonist. At sub‑therapeutic doses it’s explored for chronic pain and autoimmune conditions because it offers analgesia without full opioid activation.
Gabapentin is an anticonvulsant that’s widely used for neuropathic pain and fibromyalgia. It doesn’t target opioid receptors but modulates calcium channels to calm nerve firing.
Acetyl‑L‑carnitine is a nutritional supplement that supports mitochondrial function and has shown modest benefit in neuropathy and MS fatigue.
Cannabidiol (CBD) is a non‑psychoactive cannabinoid. It interacts with the endocannabinoid system, which indirectly influences opioid pathways and inflammation.
Head‑to‑Head Comparison
| Attribute | Low Dose Naltrexone | Naloxone (low dose) | Buprenorphine (micro‑dose) | Gabapentin | Acetyl‑L‑carnitine | CBD |
|---|---|---|---|---|---|---|
| Primary Mechanism | Transient opioid‑receptor blockade → endorphin rebound | Short‑acting opioid blockade | Partial opioid agonism | Calcium‑channel modulation | Enhances mitochondrial energy production | Endocannabinoid system modulation |
| Typical Dose | 1‑4.5 mg daily | 0.1‑0.4 mg daily (off‑label) | 0.1‑0.5 mg daily | 300‑1800 mg daily | 500‑2000 mg daily | 15‑50 mg daily |
| FDA Approval for Indication | Approved for opioid/alcohol dependence (high dose) - off‑label for LDN | Approved for overdose reversal - off‑label for low dose | Approved for opioid dependence - off‑label for micro‑dose | Approved for seizures & post‑herpetic neuralgia | Not FDA‑approved for neurological use (dietary supplement) | Not FDA‑approved for medical use (dietary supplement) |
| Common Uses | Autoimmune, chronic pain, fatigue | Investigational immune modulation | Chronic pain, mood disorders | Neuropathic pain, fibromyalgia | MS fatigue, peripheral neuropathy | Anxiety, pain, sleep |
| Side‑Effect Profile | Mild insomnia, vivid dreams | Rapid withdrawal if combined with opioids | Constipation, mild sedation | Dizziness, weight gain | Rare GI upset | Dry mouth, drowsiness |
Decision Criteria - How to Pick the Right Option
When you sit down with your doctor, ask yourself these questions:
- What’s the primary goal? If you’re targeting immune regulation, LDN or low‑dose naloxone are the front‑runners. For pure neuropathic pain, gabapentin or CBD might be more direct.
- How tolerant are you to off‑label use? LDN and low‑dose naloxone are off‑label in most countries, meaning you’ll need a physician comfortable with that risk.
- Do you have existing opioid exposure? Combining high‑dose opioids with an antagonist can precipitate withdrawal. Buprenorphine or micro‑dose strategies require careful titration.
- Cost and access? Generic gabapentin is cheap; CBD oils can be pricey and vary in quality. LDN compounding can add a modest pharmacy fee.
- Side‑effect tolerance? If insomnia is a deal‑breaker, gabapentin’s sedation might be preferable. If you’re sensitive to GI upset, steer clear of high‑dose acetyl‑L‑carnitine.
Write down your priorities, then discuss them with a clinician who knows the nuances of each drug.
Practical Tips & Common Pitfalls
- Start low, go slow. For LDN, begin at 1 mg nightly and increase by 0.5 mg each week if tolerated.
- Track symptoms. Use a simple spreadsheet: date, dose, pain score, sleep quality, side effects. Patterns emerge after 6‑8 weeks.
- Beware drug interactions. LDN can interact with opioid analgesics, certain antidepressants, and immunosuppressants.
- Quality matters for supplements. Choose third‑party tested CBD and acetyl‑L‑carnitine to avoid contaminants.
- Don’t abandon standard care. LDN is rarely a stand‑alone cure; it usually complements disease‑modifying therapies.
Frequently Asked Questions
Is LDN safe for long‑term use?
Most studies report mild side effects like vivid dreams or insomnia. Long‑term safety data are limited, but many patients have used LDN for years without serious issues. Regular monitoring by a physician is recommended.
Can I take LDN with my current prescription opioids?
Generally no. Even a low dose of an antagonist can trigger withdrawal if you’re on a stable opioid regimen. Talk to your prescriber about a safe taper before starting LDN.
How quickly can I expect to feel better?
Responses vary. Some report modest improvement within 2-4 weeks, while others need 3-6 months to notice a difference. Patience and consistent dosing are key.
Is there a generic version of LDN?
The standard 50 mg naltrexone tablets are generic, but the low‑dose formulations usually require a compounding pharmacy, which can be a bit more expensive than a regular prescription.
What if LDN doesn’t work for me?
Switching to one of the alternatives-gabapentin for neuropathic pain, CBD for inflammation, or acetyl‑L‑carnitine for fatigue-may provide the needed relief. A stepwise approach, guided by a clinician, usually yields the best outcome.
Bottom line: LDN is a promising, low‑cost tool in the chronic‑illness toolbox, but it isn’t a magic bullet. Weigh its mechanism, side‑effect profile, and the evidence against alternatives like gabapentin, CBD, and buprenorphine. Armed with the comparison table and a clear set of decision criteria, you can have a focused conversation with your healthcare provider and move toward a treatment plan that actually works for you.

Abby W
October 25, 2025 AT 12:20Wow, the LDN rundown is super helpful! 😊 I’ve been dabbling with a 1.5 mg nightly dose for my MS fatigue and noticed calmer mornings.
Lisa Woodcock
November 5, 2025 AT 16:53I totally get where you’re coming from. I tried LDN after reading about it for Crohn’s, and the first few weeks were rough on my sleep, but by week 5 my gut flare‑ups were noticeably less. The key is keeping a symptom journal – it really shows patterns you might miss. Also, if you’re on other immunosuppressants, check with your doc about any subtle interactions. Good luck navigating the options!
krishna chegireddy
November 16, 2025 AT 22:25The whole LDN hype is a classic case of anecdotal worship masquerading as science. You read a handful of tiny trials, then the internet turns every patient into a guru who swears by a 3 mg capsule. Yet, the placebo effect in chronic pain is massive, and none of those studies control for that. Moreover, the pharmacodynamics of an opioid antagonist at nanodoses remain speculative – we lack robust receptor‑occupancy data. Selling LDN as a miracle cure for autoimmune diseases without large‑scale randomized trials is, frankly, irresponsible. The table you posted looks tidy, but it glosses over the fact that most alternatives have far more safety data. Gabapentin, for instance, has been studied for decades, with clear dosing guidelines and known side‑effect profiles. CBD’s regulatory status is a mess, but at least there’s a growing body of peer‑reviewed work. Then there’s the issue of compounding pharmacies: they charge extra, and quality control varies wildly, meaning you might get a 0.5 mg dose instead of the intended 1 mg. Also, patients often ignore the warning about concurrent opioid use – even low‑dose antagonists can precipitate withdrawal, leading to a cascade of complications. In short, LDN is an interesting pharmacologic curiosity, but portraying it as a first‑line off‑label option feels like marketing hype rather than evidence‑based medicine.
Brett Witcher
November 28, 2025 AT 03:57The summary table is a nice quick‑reference, especially for busy clinicians. It clearly highlights dosage ranges and primary mechanisms, which can be confusing otherwise. One thing to watch is the side‑effect overlap – many patients report vivid dreams with LDN, similar to low‑dose naloxone. Overall, the comparison helps frame a conversation with your doctor.
Benjamin Sequeira benavente
December 9, 2025 AT 09:30Exactly, and if you’re already on a pain regimen, micro‑dosing buprenorphine can give you that analgesic lift without the heavy sedation of gabapentin. Just remember to taper slowly and monitor for constipation.
Jennifer Stubbs
December 20, 2025 AT 15:02While the optimism around LDN is commendable, the data pool is still shallow. Most studies are open‑label, small‑sample, and lack long‑term follow‑up. That said, the safety profile appears mild compared to many immunosuppressants. It’s worth a trial if you’ve exhausted first‑line options, but keep realistic expectations and document outcomes rigorously.
Abhinav B.
December 31, 2025 AT 20:34Totally agree – a solid diary is your best friend. Plus, don’t forget to double‑check supplement purity; cheap acetyl‑L‑carnitine can be contaminated.
Deborah Galloway
January 12, 2026 AT 02:07I love how this post breaks down the options without jargon. If you’re feeling overwhelmed, start with the one that matches your main symptom – pain, fatigue, or inflammation – and see how you feel after a few weeks. Remember, you’re not alone in this journey, and many online communities share dosage tips that can be lifesavers.
Charlie Stillwell
January 23, 2026 AT 07:39Great, another miracle pill.
Ken Dany Poquiz Bocanegra
February 3, 2026 AT 13:11Maybe, but evidence matters more than hype.
Tamara Schäfer
February 14, 2026 AT 18:44Philosophically speaking, we often chase the next ‘quick fix’ without considering the underlying systemic imbalance. LDN, like many off‑label agents, forces us to ask whether we’re treating symptoms or the root cause. If the immune reset you’re after is truly the goal, perhaps a holistic approach – diet, stress management, and targeted supplementation – works synergistically with any pharmacologic tool.
Tamara Tioran-Harrison
February 26, 2026 AT 00:16Indeed, an overly formal tone merely masks the lack of substantive data.