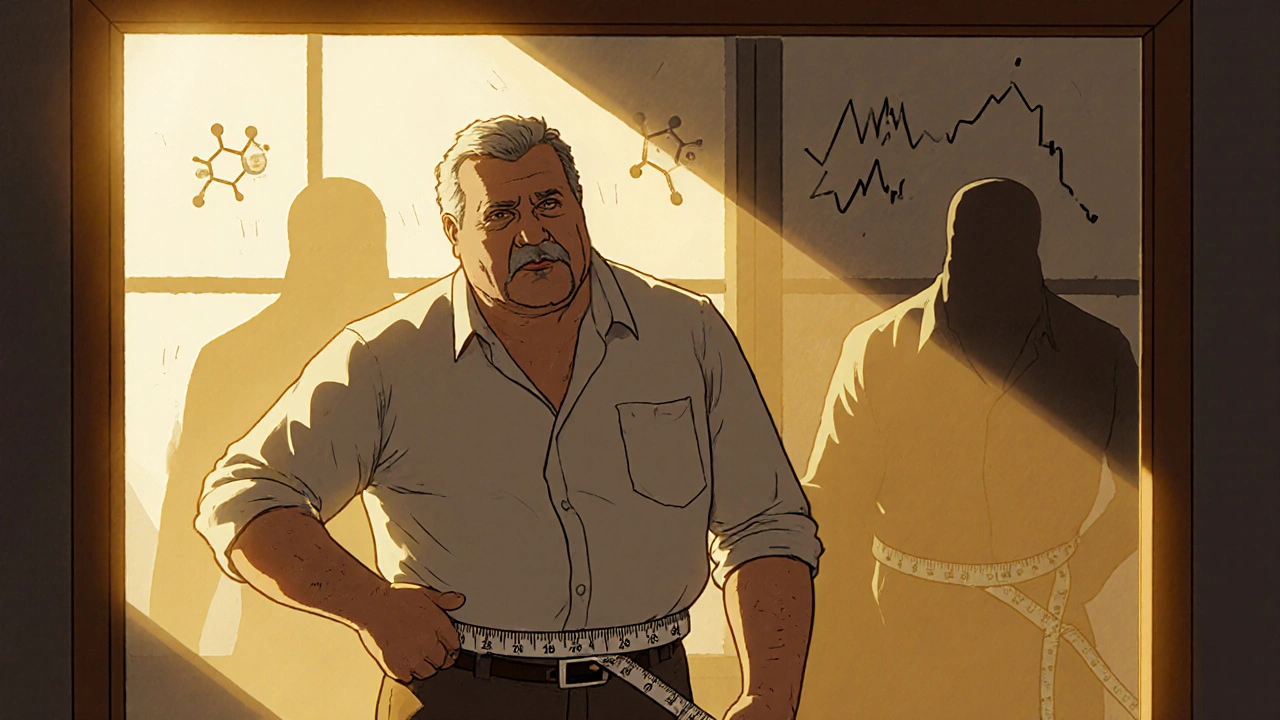
If you’ve ever been told your waist is too big, your triglycerides are high, or your blood sugar is borderline, you might’ve been handed a diagnosis you didn’t ask for: metabolic syndrome. It’s not a disease you can point to on a scan. It’s not something you feel right away. But it’s a warning sign - loud and clear - that your body’s metabolism is out of balance. And if you’re not doing anything about it, you’re walking toward type 2 diabetes or a heart attack without even realizing it.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t one problem. It’s a group of at least three out of five specific health issues that happen together. These aren’t random. They’re connected by one invisible thread: insulin resistance. That’s when your muscle, fat, and liver cells stop responding properly to insulin, the hormone that tells your body to use sugar for energy. So your pancreas pumps out more insulin to compensate. Eventually, it can’t keep up. Blood sugar rises. Fat builds up. Blood pressure creeps up. And your good cholesterol drops. The big three players in this mess? Waist size, triglycerides, and glucose control. If you’ve got problems with all three, you’re in the danger zone.Waist Size: The First Red Flag
You can’t hide abdominal fat. It doesn’t care how fit your arms or legs look. If you’ve got a belly that sticks out - especially when you’re standing - your body is sending signals you can’t ignore. According to the American Heart Association and the National Heart, Lung, and Blood Institute, men with a waist over 40 inches (102 cm) and women over 35 inches (88 cm) are flagged for metabolic syndrome. But here’s the catch: those numbers are higher for some groups. South Asian women, for example, can start showing metabolic risks at just 31.5 inches (80 cm). Why? Because fat stored around the organs - visceral fat - is far more dangerous than fat under the skin. It releases inflammatory chemicals that mess with insulin, trigger liver fat buildup, and raise blood pressure. Research from Circulation shows that every extra 4 inches (10 cm) around your waist increases your risk of heart disease by 10%. That’s not a small bump. That’s a straight line toward trouble.Triglycerides: The Hidden Fat Bombs
Triglycerides are the main type of fat in your blood. They come from the food you eat - especially sugar and refined carbs - and from your liver when insulin resistance kicks in. Normal levels are under 150 mg/dL. Once you hit 150, you’re in the metabolic syndrome range. But here’s what most people don’t know: if your triglycerides are over 200 mg/dL, your risk of heart attack jumps even without high LDL cholesterol. This isn’t just about diet. It’s about biology. When your liver gets flooded with free fatty acids from belly fat, it starts making more triglycerides and packing them into VLDL particles. These particles float through your bloodstream, clogging arteries and lowering your HDL (good cholesterol). That’s why someone can have normal LDL but still be at high risk - their triglycerides are the silent killer. The American Heart Association says limiting added sugar to less than 10% of your daily calories and cutting alcohol to one drink a day for women and two for men can make a huge difference. Prescription omega-3s help if levels are above 500 mg/dL, but most people don’t need meds. They need to stop drinking soda and start eating whole foods.Glucose Control: The Early Warning System
Fasting blood sugar above 100 mg/dL is the third key sign. That’s not diabetes yet. That’s prediabetes. And it’s your body screaming for help. The Diabetes Prevention Program - one of the most important studies in modern medicine - showed that people with fasting glucose between 100 and 125 mg/dL had a 5% to 10% chance each year of developing full-blown type 2 diabetes. But here’s the good news: those same people who lost 5% to 7% of their body weight and walked 150 minutes a week cut their risk by 58%. That’s not luck. That’s reversing insulin resistance. Most people think glucose control means cutting out sugar. It’s more than that. It’s about how your body handles carbs. Refined grains, white rice, fruit juices, even some “healthy” granolas spike blood sugar fast. Your body responds with insulin, which stores the excess as fat - especially around your belly. That’s the cycle: high carbs → high insulin → fat storage → worse insulin resistance → higher glucose.
Why These Three Are Connected
It’s not a coincidence that these three things show up together. They feed each other. Belly fat → releases chemicals → makes liver and muscles resistant to insulin → liver makes more triglycerides → blood sugar rises → pancreas works harder → fat keeps building → insulin gets weaker. It’s a loop. And it gets worse over time. The more triglycerides you have, the more they interfere with insulin signaling. The higher your blood sugar, the more your body stores fat. The bigger your waist, the more inflammation you have - which makes everything worse. Studies from Washington University show that high triglycerides cause lipotoxicity - fat poisoning in cells - which directly damages insulin receptors. So you’re not just gaining weight. You’re breaking your body’s ability to manage energy.Who’s at Risk?
You don’t have to be overweight to have metabolic syndrome. Some people with normal BMI still have a big waist and high triglycerides. That’s called TOFI - thin on the outside, fat inside. It’s common in South Asian, Hispanic, and Indigenous populations, who develop metabolic problems at lower weights than Caucasians. Age matters too. About 22% of adults aged 20-39 have it. By 60, that number jumps to nearly 50%. But it’s not just aging. It’s lifestyle. Sitting too much. Eating too many processed foods. Sleeping poorly. Stressing too hard. These aren’t just “bad habits.” They’re metabolic disruptors.What You Can Do - Right Now
The good news? Metabolic syndrome is reversible. You don’t need surgery. You don’t need a miracle drug. You need to change how you live.- Move more. Aim for 150-300 minutes of brisk walking, cycling, or swimming a week. You don’t need to run a marathon. Just keep moving.
- Eat real food. Focus on vegetables, lean proteins, whole grains, nuts, seeds, and healthy fats like olive oil and avocado. Cut out sugary drinks, white bread, pastries, and processed snacks.
- Try the Mediterranean diet. The PREDIMED trial showed it cut heart attacks by 30% in high-risk people. It’s not a diet - it’s a way of eating that’s been around for centuries.
- Drop alcohol. Even one drink a day can raise triglycerides. Two drinks? That’s a red flag.
- Sleep and stress manage. Poor sleep and chronic stress raise cortisol, which increases belly fat and blood sugar. Aim for 7-8 hours. Try breathing exercises or walking in nature.
When Medication Might Help
Lifestyle is the first and most powerful tool. But sometimes, you need help.- Metformin is often prescribed for prediabetes. It improves insulin sensitivity and can delay or prevent type 2 diabetes.
- Fibrates or high-dose omega-3s can lower triglycerides if they’re above 200 mg/dL and lifestyle isn’t enough.
- ACE inhibitors or ARBs help lower blood pressure and may improve insulin sensitivity.
The Bigger Picture
By 2030, the World Health Organization predicts half of all adults in developed countries will meet the criteria for metabolic syndrome. That’s not inevitable. It’s a choice - as a society and as individuals. This isn’t about looking a certain way. It’s about staying alive. About not needing insulin shots. About not having a heart attack at 55. About being able to play with your kids or grandkids without getting winded. Your waist size, triglycerides, and glucose levels aren’t just numbers on a lab report. They’re your body’s way of telling you: change now, or pay later.What to Ask Your Doctor
If you’re worried, don’t wait. Bring up these questions:- “Do my waist size, triglycerides, and fasting glucose suggest metabolic syndrome?”
- “Should I get a TyG index test? That’s triglycerides times glucose - it shows insulin resistance better than any single number.”
- “What’s my 10-year risk of heart disease or diabetes?”
- “Can we start with lifestyle changes before medication?”
Can you have metabolic syndrome even if you’re not overweight?
Yes. Some people have normal BMI but carry fat deep inside their abdomen - called visceral fat. This is often called TOFI - thin on the outside, fat inside. These individuals can have high triglycerides, elevated blood sugar, and insulin resistance, meeting all the criteria for metabolic syndrome. Waist circumference is a better indicator than BMI alone.
Is metabolic syndrome the same as prediabetes?
No. Prediabetes means your blood sugar is higher than normal but not yet diabetic. Metabolic syndrome includes prediabetes as one of its five components, but it also requires at least two other issues - like high waist size and high triglycerides. You can have prediabetes without metabolic syndrome, but most people with metabolic syndrome have prediabetes.
How quickly can metabolic syndrome be reversed?
Improvements can start in as little as 2-4 weeks with consistent lifestyle changes. Triglycerides often drop within days of cutting sugar and alcohol. Waist size may shrink slowly, but even a 1-inch reduction can improve insulin sensitivity. Most people see significant improvements in all markers within 3-6 months of sticking to a healthy diet and regular movement.
Do I need to take medication for metabolic syndrome?
Not always. Lifestyle changes - especially weight loss - are the most effective treatment. Medications like metformin, fibrates, or blood pressure drugs may be added if your numbers are very high or if you’re at high risk for heart disease. But no pill replaces losing weight, moving more, and eating real food. Many people reverse their diagnosis without any meds.
What’s the TyG index and why is it important?
The TyG index stands for Triglyceride-Glucose index. It’s calculated using this formula: Ln [fasting triglycerides (mg/dL) × fasting glucose (mg/dL) / 2]. It’s a simple, low-cost way to estimate insulin resistance without special tests. Studies show it’s a better predictor of metabolic syndrome than any single value. A TyG index above 8.5 suggests significant insulin resistance. Many doctors now use it alongside traditional markers.

Ryan Everhart
November 13, 2025 AT 16:42So let me get this straight - we’re diagnosing a whole syndrome based on three numbers and a tape measure? Cool. I’ll just stop looking in the mirror and let my lab results decide my worth. 🤷♂️
Also, why is everyone acting like this is new? My abuela in Puerto Rico ate rice and beans her whole life and never saw a glucose meter. Maybe the problem isn’t our bodies - it’s the food industry selling us poison in neon packaging.
David Barry
November 14, 2025 AT 13:58Let’s not romanticize this. Metabolic syndrome isn’t a ‘warning’ - it’s a death sentence with a 5-year grace period. The data’s clear: visceral fat = chronic inflammation = endothelial dysfunction. You think walking 150 minutes a week fixes that? Nah. It slows the rot. Real reversal? Only happens when you obliterate fructose, eliminate processed carbs, and sleep 7+ hours. No exceptions. No ‘healthy’ granola. No ‘moderation.’
And stop blaming aging. It’s sedentary lifestyles and corporate food lobbying. Period.
Alyssa Lopez
November 15, 2025 AT 12:47OMG I JUST REALIZED I’M PROBABLY IN THE DANGER ZONE 😭
My waist is like 38 inches but I’m only 140 lbs?? How is that even possible?? I eat kale and drink green tea!!
Also I heard the TyG index is like the new HbA1c but like… what if I don’t wanna know?? I’m scared now. Someone send help. Or at least a keto meal plan.
PS: I think this is why my doctor keeps giving me metformin but never explains why. #MetabolicSindrome #TOFI #HelpMe
Alex Ramos
November 16, 2025 AT 06:09Biggest myth: you need to ‘go all in’ to fix this. Nah. Start with one thing.
I cut out soda. Just that. No fancy diets. No gym membership. Just water. And guess what? My triglycerides dropped 80 points in 6 weeks.
Then I started walking after dinner. 20 minutes. Just me, my dog, and the sunset. No podcast. No music. Just breathing.
Now my fasting glucose is 92. I’m not ‘cured’ - but I’m not on the path to diabetes anymore.
You don’t need to be perfect. You just need to start. And keep showing up. 💪😊
Also - if you’re reading this and feel overwhelmed? You’re not alone. DM me. I’ll send you my 3-step starter list. No judgment.
edgar popa
November 16, 2025 AT 13:56waist size > bmi any day. i had a doc tell me i was ‘fine’ cause i was skinny. then i got my waist measured and he went ‘oh.’
cut out juice. cut out bread. walk 10 min after every meal. that’s it. no magic.
2 months later i lost 4 inches. no scale needed. jeans fit better. that’s the win.
Eve Miller
November 16, 2025 AT 15:32It is deeply irresponsible to suggest that ‘lifestyle changes’ are sufficient for everyone. Metabolic syndrome is a systemic metabolic disorder rooted in genetic predisposition, epigenetic triggers, and environmental toxicants - not poor willpower. To imply that losing five percent of body weight is a panacea is not only scientifically inaccurate, it is morally negligent.
Those who have been diagnosed with metabolic syndrome - particularly those with a family history of type 2 diabetes - require medical supervision, not platitudes about ‘walking more’ and ‘eating real food.’
And while we’re at it: the term ‘thin on the outside, fat inside’ is a euphemism for visceral adiposity. Let’s use precise language, not feel-good jargon.
Chrisna Bronkhorst
November 17, 2025 AT 01:13South Asians get screwed by Western guidelines. My cousin, 5’5”, 130 lbs, waist 30 inches - flagged for metabolic syndrome. Meanwhile, his white coworker, 6’0”, 220 lbs, waist 42 inches - ‘oh you’re just big, not sick.’
It’s not about weight. It’s about fat distribution and insulin sensitivity. And the research? It’s all based on white male cohorts.
So yeah - your ‘normal’ is not my normal. And your ‘danger zone’ is built on colonial science. Fix the system, not the patient.
Amie Wilde
November 17, 2025 AT 14:44My mom had this. Didn’t know it. Got a heart attack at 58.
I started walking. Cut soda. Got my waist measured. 34 inches.
Still not perfect. Still stressed. Still eat pizza sometimes.
But I’m not waiting for a crisis to care.
Small steps. That’s all.
Gary Hattis
November 18, 2025 AT 20:39Back home in Nigeria, we used to say ‘the belly is the first to speak’ - meaning if your stomach grows, your health is whispering. No labs needed.
But now? Everyone’s chasing pills and apps. Meanwhile, our grandmas cooked yam with palm oil, ate fresh fish, and walked 5 miles to market. No ‘Mediterranean diet’ - just food that came from the ground, not a factory.
Maybe the answer isn’t in a new study. Maybe it’s in remembering how our ancestors lived.
Also - if you’re reading this and you’re not from a Western country? Don’t let them make you feel broken because you don’t look like their ‘ideal’ body. Your body knows how to heal. You just have to stop feeding it lies.