If you've ever left the doctor's office clutching a prescription for Plavix and a whole list of questions buzzing through your head, you're not alone. Being told your blood needs a "thinner" to keep your heart safe sounds simple—until you realize it's not aspirin, your diet might matter, and random nosebleeds could suddenly mean something big. Plavix has been on the market for decades and has already changed—and saved—countless lives. But the behind-the-scenes action in your bloodstream, the risks you’re balancing every day, and the fine print your pharmacy slips into the bag? That's the stuff that actually shapes what happens next. Let’s peel back the mystery and get clear on what really matters with Plavix.
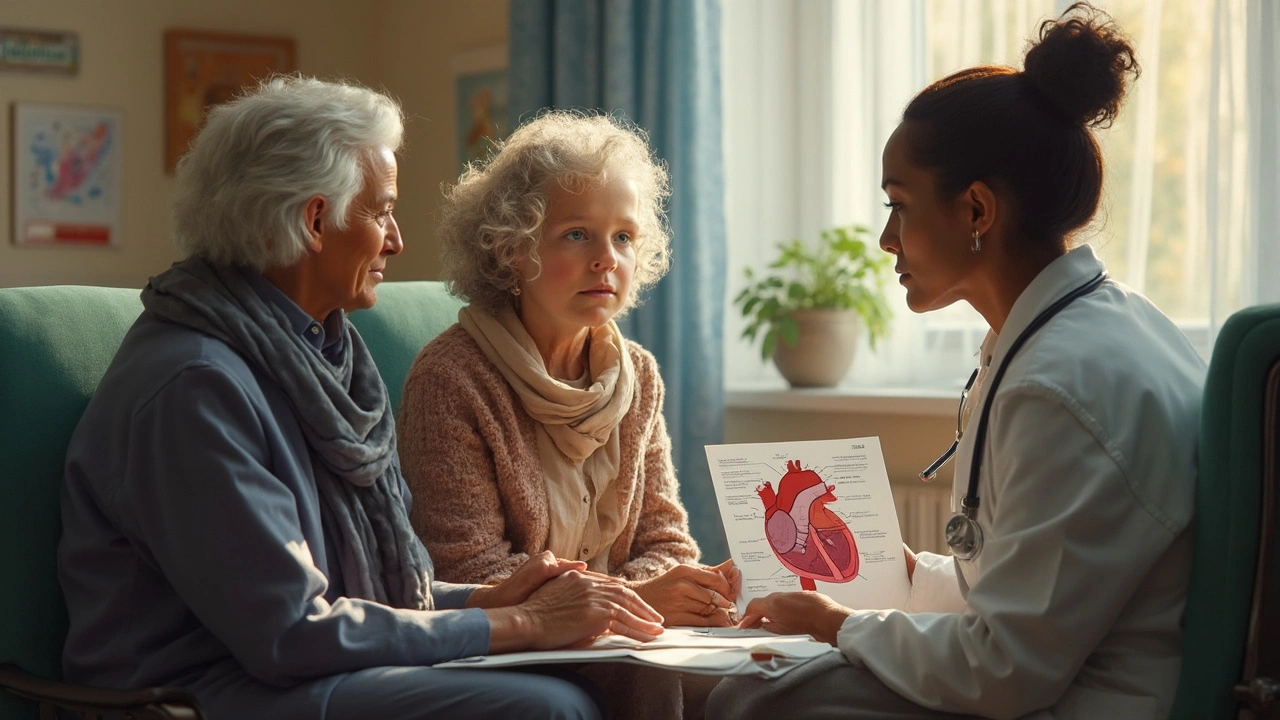
What Plavix (Clopidogrel) Does and Why It’s Prescribed
The moment you hear "Plavix"—which is the brand name for clopidogrel—think "preventing clots." That’s its job, plain and simple. It’s not thinning your blood like water; it’s blocking special cells called platelets from clumping together. Normally, platelets help you stop bleeding, but when you have certain heart conditions, your body can overreact and form dangerous clots inside your arteries. Those clots can block blood flow, leading to a heart attack or stroke. Plavix helps keep that risk way down for people who've already had an event like a heart attack, have clogged arteries, or have metal stents keeping their arteries open.
Doctors often prescribe Plavix for folks who've just had a stent put in after a procedure called angioplasty, or for people who can’t take aspirin, or need something even stronger. It’s also used for people with something called Peripheral Artery Disease (that’s when leg arteries get gummed up just like those in your heart) and for people who’ve had certain strokes or mini-strokes. Do you have atrial fibrillation—an irregular and sometimes fast heartbeat? Plavix is rarely the first-line option there, but in some cases, it comes into play when other blood thinners aren’t a fit.
Here’s what has kept Plavix in doctor’s good graces for so long: even though it’s now a generic (which means it’s a lot cheaper and covered by insurance), research still shows it’s effective and safe when used the right way. The CURE trial—a huge study—proved Plavix plus aspirin reduced the risk of another heart event better than aspirin alone. Not a magic shield, but a measurable difference: about 20% lower risk for new heart attacks or strokes in certain people, especially after stent placement.
Let’s talk numbers: over 20 million prescriptions for Plavix get filled every year in the U.S. alone. Its reach is massive. Not in a “TV commercial” sense, but in the real-world, "I just want to keep my heart beating" sense. Yet, there’s an art to getting it right. The standard dose is 75 mg a day, but you might see a high "loading dose" first, especially right after a big cardiac event.
Bottom line: If your doctor says you need Plavix, they're betting the risk of a clot in your future is bigger than the risk of you bleeding too easily now. The benefits stack up quickly—when taken as directed, and when you know what signs to look for if things don’t go as planned.
Side Effects, Risks, and Real-World Tips for Staying Safe
No one loves reading the side effects section, but skipping it with Plavix is a bad idea. Since it slows your platelets, the number one concern is excessive bleeding. Not just big things like cuts that won't stop, but smaller stuff: nosebleeds that surprise you, bruises that show up out of nowhere, or gums bleeding when you brush your teeth. In rare cases (seriously rare—about 1 in 10,000), it can cause a dangerous condition called TTP (thrombotic thrombocytopenic purpura). This hits hard, with symptoms like sudden purple spots on your skin, confusion, fever, or yellowing of the eyes. If you get any of those, you have to head to the ER, ASAP.
Next up: interactions. Mixing Plavix with other meds—especially things like ibuprofen, naproxen, or certain antidepressants—can crank up your bleeding risk. Even natural supplements like ginkgo or ginger can mess with how well your platelets work. Always, always share your full med list every time you see a new doctor or even a dentist. Just one missed detail can change your risk level.
Got surgery coming up—anything from a tooth pull to a knee replacement? Your healthcare team will help you weigh the bleeding risk versus the risk of developing a clot after you stop Plavix. Sometimes you’ll be told to stop Plavix 5-7 days before a procedure. Never stop it on your own—quitting cold turkey, especially soon after a stent, can lead to a clot in the stent itself. That’s a full-blown emergency.
Curious about drinking? Light alcohol isn’t totally off-limits, but heavy drinking makes bleeding much worse. Find a balance with your routines—a glass of wine with friends is usually fine, but check with your doc if you’re not sure.
Diet won’t usually interact with Plavix itself (it’s not like warfarin, where leafy greens make a big difference), but you should pair it with food if it bothers your stomach. Otherwise, just take it at the same time daily so you never skip a dose. Miss one? Don’t double up—just take your next pill when you remember.
People have a lot of questions about side effects. For example, why are you bruising more, and is it “normal”? Some bruising is almost expected—you might see blue-black or yellow-green marks after bumping into furniture. If you ever see blood in your pee or stool, vomit that looks like coffee grounds, or any sort of uncontrolled bleeding, call your doctor (or head to urgent care). Not everyone gets these issues—some go years on Plavix with barely any blips—but being prepared beats being surprised.
Here's a quick breakdown of common and rare side effects:
| Side Effect | How Often? | What To Do? |
|---|---|---|
| Easy bruising | Common (up to 1 in 4) | Usually harmless. Monitor spots; see doctor if they multiply or spread fast. |
| Nosebleeds & Gum Bleeding | Moderate | Switch to soft toothbrush; seek advice if it becomes frequent. |
| Weakness/Fatigue | Less common (about 1 in 20) | Check for anemia during routine blood tests. |
| TTP (see above!) | Very rare | Get emergency care immediately. |
| Allergic rash | Rare | Stop and seek medical attention. |
If you want to get proactive, keep a journal with any weird bruises, nosebleeds, or odd symptoms. That record can help your doctor tweak your dose or figure out if another med is causing problems. If you’re a fall risk at home, now’s the time to “babyproof” your living space—clear the hallways, install grab bars, and pick up a night light. The small stuff makes a big difference if you’re bleeding more easily on Plavix.

Alternatives, New Research, and Everyday Survival Tips
People always ask if there’s a "better" or "safer" blood thinner than Plavix. The answer? Maybe, maybe not; it really depends on your situation. The most common switch you’ll hear about is to newer drugs like ticagrelor (Brilinta) or prasugrel (Effient). Both block platelets even more powerfully than Plavix, but they’re more expensive, and some people just don’t tolerate them as well (think stubborn shortness of breath or dangerous drops in white blood cells). Plavix’s big advantage? It’s generic, widely covered, and well-studied—thousands of patients, years of follow-up, and heaps of real-world data. It’s the "Honda Civic" of blood thinners: maybe not the flashiest, but reliable, effective, and rarely lets you down if you use it the right way.
Why do some people respond to Plavix and others don’t? Genetics is a big deal here. About 1 in 3 people of Asian descent, and 1 in 5 people worldwide, have genetic tweaks (CYP2C19 variants) that keep them from fully activating Plavix in their bodies. Some big hospitals now run quick cheek swabs before starting therapy, but most folks will never be tested. If you’ve had a clot while faithfully taking Plavix, ask your doctor about these gene tests or if a med switch is smart for you.
If you vet the research, a lot of headlines zero in on dual therapy: Plavix plus aspirin. For most people after a heart attack or stent, that combo sticks around anywhere from 3 months to 1 year, depending on your risk of clots versus risk of bleeding. After that, doctors usually drop one (often aspirin), and keep you on the other long-term.
Let’s get real about sticking with Plavix—adherence is where folks slip up, and skipping just a few days at the wrong time can undo all your hard work. Set a phone alarm, use a pillbox, or ask a family member to check in on you—whatever works. Some people haul their bottle of Plavix to family gatherings during holiday season to show everyone they're not being "difficult," they're staying alive. If you travel a lot, carry your prescription label and a doctor’s note; security at airports sometimes asks about unusual pills.
- Trouble swallowing pills? Plavix shouldn’t be crushed or split without asking your pharmacist, since the pill coating controls how it’s absorbed.
- Pregnant or breastfeeding? Plavix hasn’t been studied enough for confident use in pregnancy, so tell your doctor if there’s a chance you could be pregnant.
- Trying to balance Plavix with sports or outdoor activities? Wear sturdy shoes outdoors, slap on gloves for yard work, and use a helmet on your bike—just in case.
- Feeling isolated or worried? Ask your pharmacy about local support programs (sometimes run by hospitals or heart health groups); it helps to hear from people living on this med every day.
What about diet or special foods? Grapefruit juice isn’t a big concern here (unlike some other heart meds), but do let your pharmacist know about heavy herbal supplement use. Stick to heart-healthy staples: colorful veggies, lean proteins, and not-too-much salt or sugar. Work with a dietitian if the rest of your med list starts interfering with your appetite.
And finally: never underestimate the power of a small notebook or reminder app. Write down every weird symptom, every question, every skipped dose. Show it to your doc when you visit. You’re not bothering them. You’re giving them the real info they need to keep you safe and healthy. Plavix works best when you—not just your arteries—stay in the game, alert and informed.

Sunthar Sinnathamby
May 30, 2025 AT 12:13Hey everybody, I get how intimidating all that medical jargon can feel, especially when you’re staring at a prescription for Plavix and wondering what the heck it actually does. The good news is it’s designed to keep your blood from forming dangerous clots, which can mean the difference between a quick recovery and a life‑threatening event. Stick to the schedule your doctor gave you and don’t skip doses – consistency is key. If you ever feel a weird bruise or a nosebleed that won’t quit, note it down and let your healthcare team know right away. Stay proactive, stay positive, and keep looking out for each other – together we can manage this thing.
Catherine Mihaljevic
May 30, 2025 AT 13:36I bet the drug companies deliberately hide the real bleeding risks from us.
Michael AM
May 30, 2025 AT 15:00Plavix can be a lifesaver for many heart patients. It blocks platelets from clumping so clots are less likely. You should never stop it without talking to your doctor. If you miss a dose take the next one at the usual time. Do not double up because that raises bleeding risk. Common side effects include bruising nosebleeds and gum bleeding. Those are usually harmless but watch if they become frequent. If you see blood in your stool or vomit call emergency services. Over the counter painkillers like ibuprofen can increase bleeding. Ask your pharmacist before adding any supplement. Some people have a genetic variant that makes the drug less effective. A simple cheek swab can tell you if that’s the case. If you have that variant talk to your doctor about alternatives. Staying consistent with the pill and keeping a symptom diary helps. Remember the benefit of preventing a heart attack far outweighs occasional bruises.
Rakesh Manchanda
May 30, 2025 AT 16:23Allow me to elucidate: while Plavix is indeed a workhorse in the cardiology arena, one must not overlook the nuanced pharmacodynamics that distinguish it from its contemporaries. The molecule’s reliance on CYP2C19 activation introduces inter‑patient variability that can be both fascinating and clinically salient. Moreover, when juxtaposed with newer agents such as ticagrelor, one discerns a trade‑off between efficacy and tolerability. Nevertheless, for the majority of patients, Plavix remains a pragmatic, cost‑effective solution that has stood the test of time.
Erwin-Johannes Huber
May 30, 2025 AT 17:46It’s really encouraging to see everyone sharing their experiences – that collective knowledge is priceless. If you’re ever unsure, a quick chat with your pharmacist can clarify many of those supplement interactions. Keep that symptom journal handy; it makes follow‑up visits far more productive.
Tim Moore
May 30, 2025 AT 19:10Dear community, I would like to express my sincere appreciation for the diverse perspectives presented herein. It is evident that Plavix occupies a pivotal role within contemporary cardiovascular therapeutics, particularly when cost considerations are paramount. Nonetheless, one must remain vigilant regarding pharmacogenomic variations that may attenuate therapeutic response. I encourage all participants to consult their healthcare providers for personalized counsel, thereby ensuring optimal and safe utilization of this medication.
Erica Ardali
May 30, 2025 AT 20:33In the grand theater of mortality, Plavix stands as both protagonist and antagonist – a paradox that mirrors the human condition itself. To swallow a pill is to sign a fragile pact with fate, trusting chemistry over chaos. Yet, amidst the bruises and the quiet triumphs, we discover that mortality is not a curtain but a dialogue.