Immunosuppressant Side Effects: What You Need to Know About Risks and Management
When your body’s immune system is turned down on purpose, it’s usually because you’re taking immunosuppressant drugs, medications designed to reduce immune system activity to prevent organ rejection or control autoimmune diseases. Also known as anti-rejection drugs, these aren’t optional extras—they’re life-saving for transplant patients and people with conditions like lupus or Crohn’s disease. But every time you suppress your immune system, you’re opening the door to risks you can’t ignore.
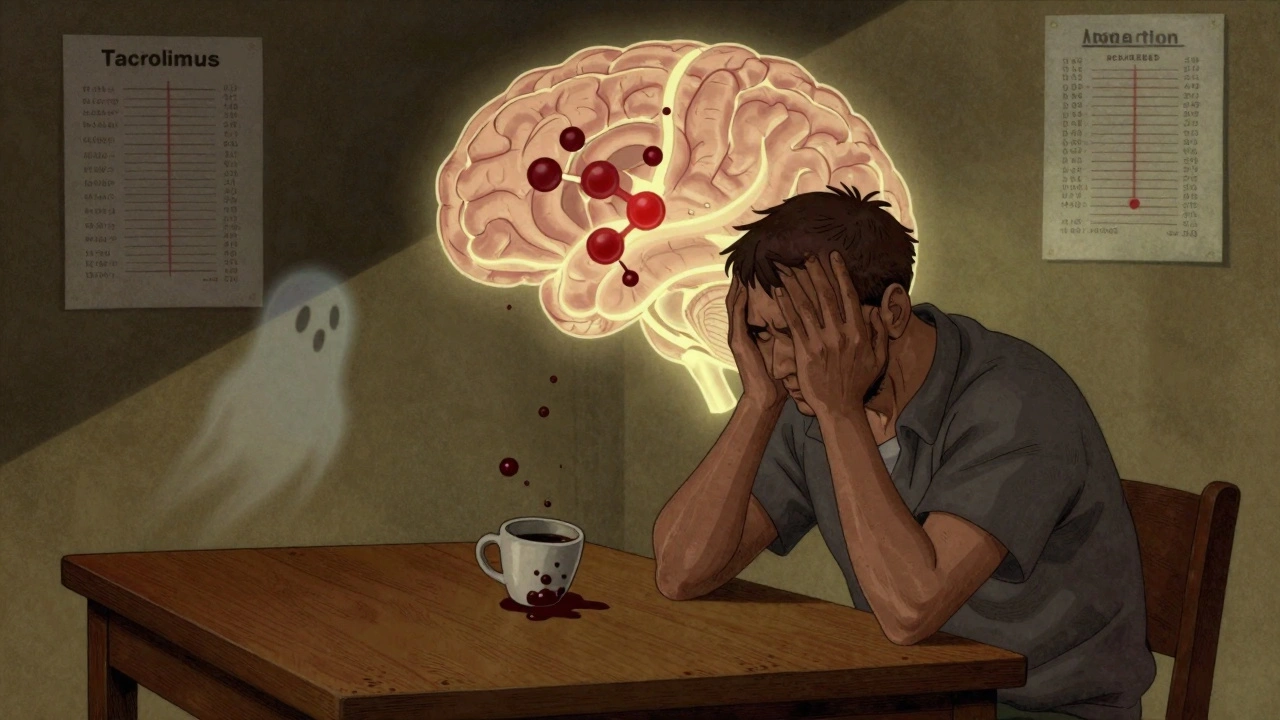
These drugs don’t just calm overactive immunity—they make you vulnerable. Infections, from common colds to deadly fungi or viruses like CMV become much more dangerous. Kidney damage, a known side effect of drugs like cyclosporine and tacrolimus can creep up slowly, often without symptoms until it’s advanced. And then there’s the long-term worry: cancer risk, especially skin cancer and lymphoma, rises because your body can’t spot and destroy abnormal cells the way it should. These aren’t rare outcomes—they’re well-documented consequences that every patient on these drugs needs to track.
It’s not just the drugs themselves. Drug interactions, like mixing immunosuppressants with grapefruit juice or certain antibiotics, can spike blood levels and turn a safe dose into a toxic one. Even something as simple as a new supplement or over-the-counter painkiller can throw off your balance. That’s why regular blood tests aren’t just routine—they’re your early warning system. And if you’re on multiple meds, you’re not just managing one condition—you’re managing a web of risks.
There’s no way around it: taking immunosuppressants means living with trade-offs. You gain protection from rejection or flare-ups, but you lose some of your body’s natural defenses. The goal isn’t to avoid these drugs—it’s to use them smartly. That means knowing the signs of trouble: unexplained fever, unusual fatigue, new skin spots, or persistent diarrhea. It means talking to your pharmacist before taking anything new. It means getting your blood checked on time, every time.
Below, you’ll find real, practical guides that cut through the noise. You’ll learn how comorbidities like diabetes or kidney disease make side effects worse, why certain drug combos are dangerous, and how to spot hidden risks in your medication routine. These aren’t theory pieces—they’re from people who’ve been there, and they tell you exactly what to watch for, what to ask, and when to act.